Ablation vs. Drugs for Ventricular Tachycardia
December 15, 2025
By Michael H. Crawford, MD
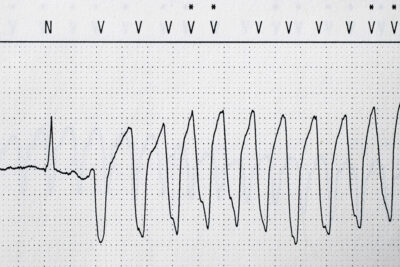
Synopsis: A sub-analysis of the VANISH2 trial, which compared catheter ablation (CA) to antiarrhythmic drug therapy for the suppression of ventricular tachycardia (VT) in patients with ischemic cardiomyopathy has shown that in the sotalol therapy group, those randomized to CA less frequently experienced the VT-based composite endpoint. Conversely, in the amiodarone group, the primary endpoint was similar in the CA- and drug therapy-randomized patients, but amiodarone produced more adverse events.
Source: Nery PB, Wells GA, Tang ASL, et al. Catheter ablation versus sotalol or amiodarone for ventricular tachycardia: A substudy of the VANISH2 trial. JACC. 2025; Sep 30. https://doi.org/10.1016/j.jacc.2025.09.1595. [Preprint].
The Ventricular Tachycardia Antiarrhythmics or Ablation in Ischemic Heart Disease (VANISH2) trial showed that first-line therapy with catheter ablation (CA) in post-myocardial infarction (MI) patients with ventricular tachycardia (VT) and ischemic cardiomyopathy resulted in a 25% reduction in the composite endpoint of death, appropriate implantable cardioverter defibrillator (ICD) shocks, VT storm, or VT below the ICD detection limit compared to antiarrhythmic drug therapy (ADT).1
This prespecified sub-analysis sought to analyze the comparative effectiveness of CA vs. ADT according to the two ADT types, sotalol and amiodarone (amio). This was a multicenter, open-label randomized controlled trial with blinded endpoint adjudication in patients with prior MI and clinically significant VT defined as VT storm, appropriate ICD shock, recurrent antitachycardia pacing (more than three episodes), or sustained VT presenting for emergent treatment that compared ADT to CA.
In 22 centers in the United States, Canada, and France, 416 patients were enrolled: 199 in the sotalol group and 217 in the amio group (mean age 67 years and 69 years, respectively). Almost all the patients were men, and the majority were white. After an average follow-up of 4.3 years, the primary composite endpoint was achieved in 46% of the CA patients and 59% of the sotalol patients (hazard ratio [HR], 0.64; 95% confidence interval [CI], 0.43-0.94; P = 0.02). In the amio subgroup, the primary endpoint was achieved in 55% of the CA patients and 62% of the amio patients (HR, 0.86; 95% CI, 0.61-1.22; P = NS).
Among the individual endpoints in the composite, in the sotalol stratum, appropriate ICD shocks occurred in 28% in the CA group and in 45% of the sotalol group (HR, 0.54; 95% CI, 0.34-0.87; P = 0.01). In the sotalol stratum, treated sustained VT below the detection rate of the ICD occurred in 2% in the CA group and 17% of the sotalol group (HR, 0.12; 95% CI, 0.03-0.51; P = 0.004). In the amio stratum, it occurred in 7% of the CA group and 16% of the amio group (HR, 0.41; 95% CI, 0.17-0.99; P = 0.05).
In the sotalol stratum, adverse events were not different between the CA group and the sotalol group. However, in the amio stratum, non-cardiac deaths were three times higher when compared to CA, pneumonia was three times higher, respiratory failure was twice as prevalent, heart failure hospitalization was 50% higher, and pulmonary fibrosis was 5% higher (vs. 0 with CA).
The authors concluded that the primary combined endpoint was less frequent in patients in the sotalol stratum with CA. In the amio stratum, the primary endpoint was similar in the CA and amio therapy groups, but adverse events were more frequent with amio.
Commentary
ICD shocks are frequent in post-MI patients; thus, ADT is warranted in many. Sotalol and amio are the most frequently used, and the VANISH2 trial treated patients with one or the other depending on patient characteristics. Sotalol has been shown to be less effective than amio but better tolerated, so it is favored in patients without severe left ventricular dysfunction, renal disease, or VT storm, whereas amio is favored in patients with severe left ventricular dysfunction and electrical storm.
Although VANISH2 showed that CA was more effective than ADT in general, this sub-analysis sought to determine the effectiveness of CA vs. ADT in the two antiarrhythmic drug stratums, since these represent two distinct patient populations.1 In the sotalol group, CA was superior to ADT. This primarily was the result of fewer episodes of appropriate ICD shocks for VT episodes below the detection rate of the ICD. In the amio group, patients randomized to CA vs. ADT had comparable rates of the primary endpoint. This primarily was because of the approximately three times more frequent rate of non-cardiac death and more frequent pulmonary and heart failure events. The non-cardiac death rates were similar in those randomized to CA in the two drug groups, but cardiovascular mortality was higher in the amio-eligible group. Not surprisingly, amio-eligible patients have more comorbidities and worse New York Heart Association class.
The results of this sub-analysis of VANISH2 suggest that more detailed clinical information than was provided by the initial report is necessary to make treatment decisions in ischemic cardiomyopathy patients with VT; namely, that CA is a better choice in patients eligible for sotalol to suppress VT. In amio-eligible patients it will be effective, but the long-term adverse effects of amio must be considered. The researchers proposed that perhaps amio could be used as a short-term bridge to CA or to stabilize the patient until their candidacy for CA, heart transplantation, or left ventricular assist device is determined.
There are limitations to the sub-analysis of VANISH2 to consider. Almost all the patients were men, and the majority were white. Women and other groups may not experience the same results. Also, the patients and providers were not blinded to the treatments, so there could be an ascertainment bias for ADT-related adverse events. In addition, less than 2% of the patients were taking sodium-glucose cotransporter 2 inhibistors and less than half were taking neprilysin inhibitors. Finally, amio was not compared to CA in the sotalol group, which is a reasonable clinical decision, whereas comparing sotatol to CA in the amio group is not.
Michael H. Crawford, MD, is Professor Emeritus of Medicine and Consulting Cardiologist, UCSF Health, San Francisco.
Reference
1. Sapp JL, Tang ASL, Parkash R, et al. Catheter ablation or antiarrhythmic drugs for ventricular tachycardia. New Engl J Med. 2025;392(8):737-747