
Treated as Aberrant SVT
September 15, 2025
By Ken Grauer, MD
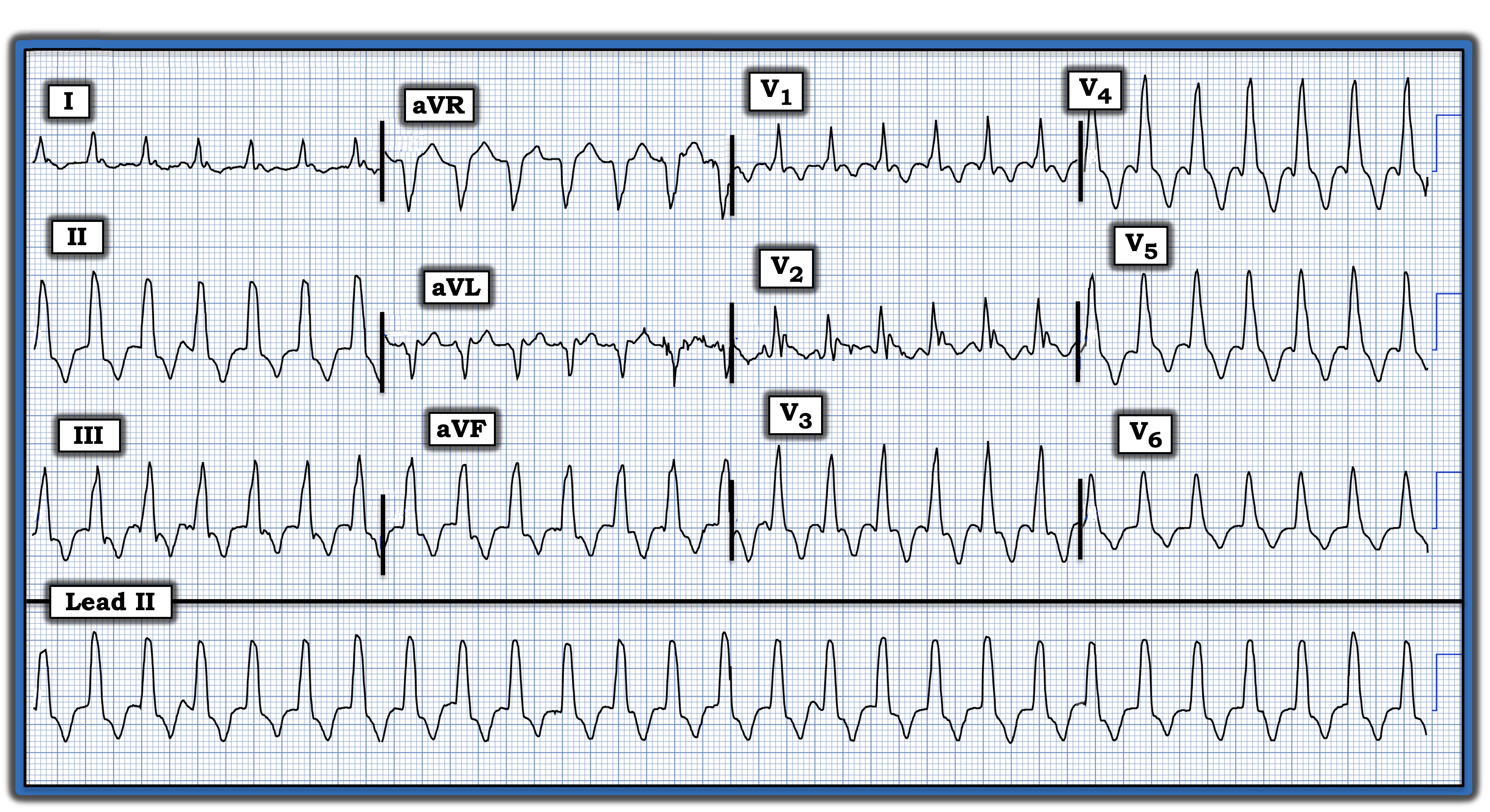
I was given this electrocardiogram (ECG) without knowing details of the history beyond that the patient was an older man who was hemodynamically stable. He was being treated on the assumption that the rhythm was a supraventricular tachycardia with QRS widening because of aberrant conduction. Do you agree with this assumption? How certain are you of your answer?
Interpretation: The “good news” is that this patient was hemodynamically stable at the time this ECG was recorded. This means that there was at least a moment of time for systematic assessment.
- The rhythm in the figure is regular at a rate of about 160 beats/minute. The QRS is wide. There is no evidence of atrial activity. This defines the cardiac rhythm as a regular wide-complex tachycardia (WCT), for which the principal differential diagnosis is between ventricular tachycardia (VT) vs. some form of a supraventricular rhythm with QRS widening because of either preexisting bundle branch block or rate-related aberrant conduction.
- Statistically, the odds that a regular WCT rhythm without clear sign of P waves will turn out to be VT are at least 80% before looking further at specific ECG features. These odds approach 90% if the patient is older and has known heart disease. Thus, the task of providers is not to “rule in” VT — but rather to assume that a regular WCT without P waves is VT until proven otherwise.
Perhaps the most helpful clue to the etiology of a regular WCT rhythm lies with assessment of QRS morphology. Is QRS morphology suggestive of some known form of conduction defect? If not — then the rhythm almost certainly is VT.
- Regarding today’s ECG, the predominantly upright QRS complex in lead V1 could be consistent with right bundle branch block (RBBB) conduction. However, the fact that all six chest leads remain predominantly (or totally) positive, and the lack of any wide terminal S wave in lateral leads I and V6, are completely against RBBB conduction.
- Today’s ECG also is inconsistent with left bundle branch block (LBBB) conduction because the QRS should be predominantly negative in anterior leads if LBBB conduction is present.
Impression: Given the complete lack of resemblance of QRS morphology in today’s tracing to any known form of conduction defect, I would estimate the likelihood of VT at greater than 95%. When in doubt in cases like this, synchronized cardioversion is advised either immediately or if cautious trial of an antiarrhythmic is unsuccessful. Fortunately for providers in today’s case, this patient spontaneously converted to sinus rhythm before further treatment was needed.
For more information about this case, visit https://tinyurl.com/KG-Blog-460.
Ken Grauer, MD, is Professor Emeritus in Family Medicine, College of Medicine, University of Florida, Gainesville.