The Cause of the ‘Burning?’
April 15, 2025
By Ken Grauer, MD
The electrocardiogram (ECG) in the figure is from a man with a new and severe “burning” chest discomfort. On seeing this ECG, the paramedic team requested activating the cath lab. Would you have done the same?
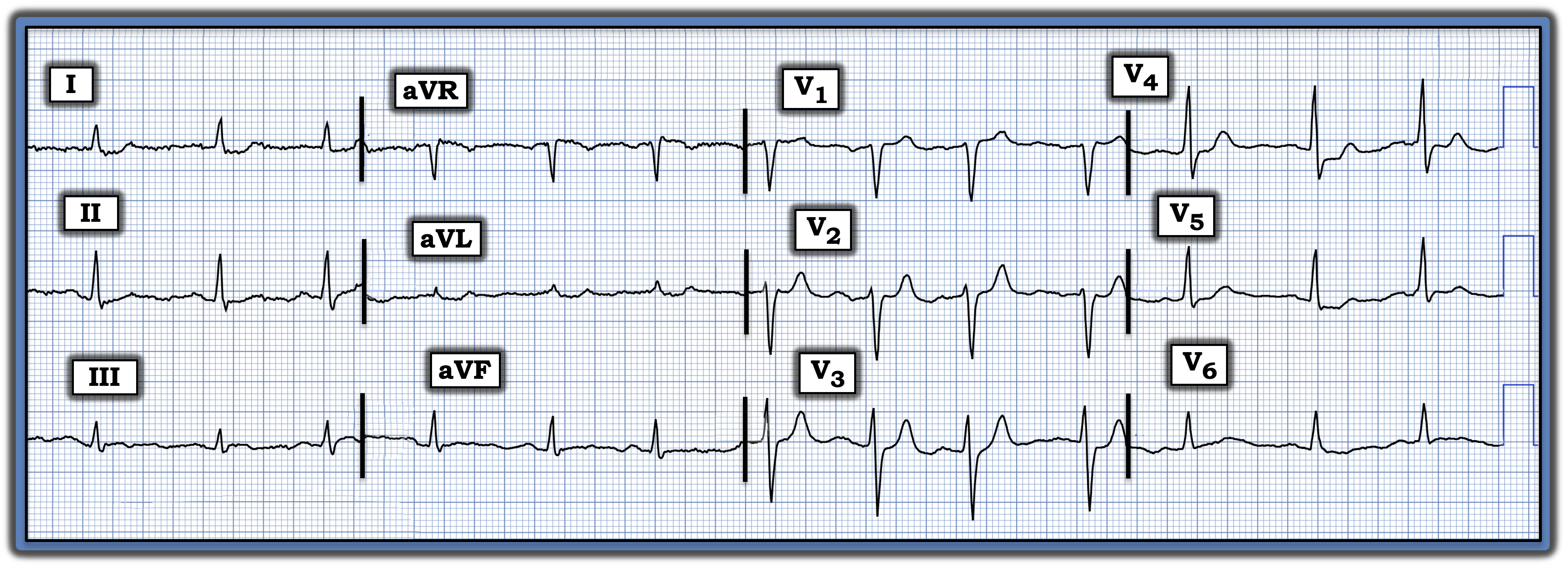
Interpretation: The ECG in the figure shows a normal sinus rhythm at ~85 beats/minute. All intervals (PR, QRS, QTc) and the axis are normal. There is no chamber enlargement. There are no Q waves, and R wave progression is normal.
The key findings are subtle-but-real ST-T wave abnormalities in a number of leads. Those, in association with the patient history, should prompt significant concern.
- Normally, there should be slight, gently upsloping ST elevation in anterior leads V2 and V3. Instead, the ST segment in lead V2 appears straightened with, if anything, a slight ST depression in neighboring lead V3. In addition, the T wave in lead V2 (if not also in lead V3) looks disproportionately taller than it should be, given R wave amplitude in these respective leads.
To emphasize, the previously noted ST-T wave changes in leads V2 and V3 are extremely subtle. That said, there can be no doubt that the ST segment straightening and depression seen in lead V4 is real and supports the validity of our suspicion regarding the subtle abnormalities noted in leads V2 and V3.
- Additional ST-T wave findings of potential concern include nonspecific ST segment flattening in multiple leads, with slight ST depression in leads I, II, and V5, and ST segment coving, with the suggestion of slight ST elevation and shallow terminal T-wave inversion in lead III.
Impression: At least one-third of all acute coronary occlusion myocardial infarctions (MI) never satisfy millimeter-based criteria for an acute ST-elevation MI (STEMI). The importance of recognizing these patients with acute occlusion-based MIs (OMIs), who do not satisfy STEMI criteria, is that they benefit equally by prompt cardiac catheterization with percutaneous coronary intervention to reperfuse the “culprit” artery that was occluded.
- In today’s patient with new chest discomfort, the findings of subtle anterior lead ST segment flattening with ST depression, in association with disproportionately taller-than-expected anterior T waves plus the ST-T wave changes seen in lead III, suggest recent infero-postero OMI. The reason that frank ST elevation is missing probably is the result of spontaneous reperfusion of the “culprit” artery.
- Prompt cardiac catheterization should be considered, especially if chest discomfort persists, if serum troponin is elevated, and/or if serial ECGs suggest ongoing evolution.
- To emphasize, in a patient such as this, the initial ECG should be repeated within no more than 15 to 30 minutes after the initial tracing, since “dynamic” ST-T wave changes may occur surprisingly soon in an actively evolving process.
- Follow-up: Acute infarction was confirmed, cardiac catheterization revealed multi-vessel disease, and the patient was scheduled for coronary bypass surgery.
Note: For more information about this case, visit https://tinyurl.com/KG-Blog-467.