Imposed Diagnostic Stewardship and Pediatric Blood Cultures
December 1, 2025
By Philip R. Fischer, MD, DTM&H
Synopsis: A children’s hospital developed a strategy to restrict indications for ordering blood cultures when supply chain problems led to a shortage of blood culture bottles. Evaluating outcomes, they realized that the imposed diagnostic stewardship preserved resources without harm to patients; they subsequently continued to impose restrictions on ordering blood cultures even when supplies were available.
Source: Vaugon E, Costales C, Assad Z, et al. Rapid diagnostic stewardship, and blood culture use in a pediatric medical center. JAMA Netw Open. 2025;8(10):e2535580.
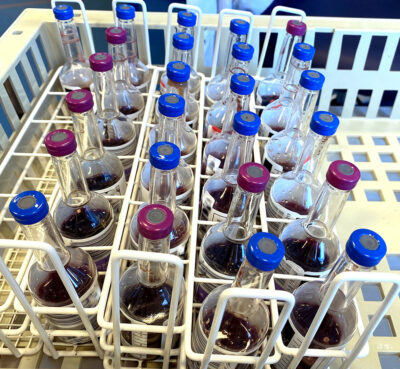
There are three main manufacturers of blood culture bottles in the United States. In June 2024, one of the three manufacturers had supply chain problems that led to eight months of decreased production. Blood culture bottles were no longer available to keep up with routine demand. Hospitals were required to institute contingency plans.
A major children’s hospital in Los Angeles chose to restrict blood culture indications and followed outcomes, comparing the 12 months prior to imposed restrictions with six months of imposed restrictions.
Aware of pending limits in availability of blood culture bottles, a multidisciplinary team was formed that included individuals with expertise in pediatric infectious disease, clinical microbiology, hematology-oncology, emergency medicine, informatics, and supply chain. They wanted to reduce the use of blood cultures while minimizing the risk to patients. They decided to limit the use of aerobic blood cultures to no more than once every 48 hours for each patient, to limit anaerobic blood cultures to no more than once each seven days, to combine/pool samples from multiple lumens of the same catheter into a single blood culture bottle, and to give physicians the prerogative to order one additional aerobic blood culture within seven days if they thought it was necessary. Electronic medical records imposed the restriction, but overrides were possible following consultation between a clinician and a microbiologist.
Blood culture positivity rates served as the primary outcome. Secondary outcomes included rates of blood culture collection, blood cultures with adequate blood volumes, lengths of hospital stay, readmission rates, and mortality rates.
There were 18,132 blood cultures (from 5,063 patient visits) sampled during the pre-intervention period and 6,449 (from 2,495 patient visits) during the period of imposed restrictions on ordering blood cultures. The median age of patients was 5.6 years.
In the emergency department, the blood culture positivity rate was 2.1% prior to restrictions, and the rate was statistically similar (with a non-significant change to 2.7%) during the months of imposed restrictions. For inpatients, the blood culture positivity rate was 1.4% prior to restrictions and a statistically similar 2% with restrictions.
There was a 24.1% decrease in the number of blood culture bottles used per 100 emergency department visits, and, in inpatient units, a 45.8% decrease in the number of blood culture bottles used per 100 inpatient days. Most of the decrease in inpatient blood culture bottle use was related to a 52.2% decrease in repeat blood cultures. The authors point out that the literature is clear that repeat blood cultures rarely are positive in patients receiving treatment for either streptococcal or anaerobic species, but they recognize that repeat cultures are positive more often with Staphylococcus aureus and yeast infections, for which follow-up culture positivity might influence decisions about the total duration of antimicrobial therapy.
Neither the overall mortality rate nor the rate of mortality related to suspected sepsis changed with restricted use of blood cultures. The length of stay was similar prior to and during the time of restricted blood cultures. The rate of readmission within seven days dropped during the period of restricted blood culture use.
The investigators reviewed the charts of 40 patients who died of suspected sepsis, 25 prior to restricted use of blood cultures and 15 during the time of restricted use. In retrospect, only one death was possibly related to a delay in obtaining a blood culture, and that patient received care during the pre-intervention period.
Patients had 26% less blood sampled each day for cultures during the intervention/stewardship period. This could represent a significant reduction in the risk of anemia for small newborns.
When blood culture bottles again became available, the investigators’ institution continued with some of the restrictions. However, they did allow repeat blood cultures within a week of positive cultures for individuals with S. aureus bacteremia or candidemia.
Commentary
Even when we think we are being judicious with microbiologic testing, supply chain challenges have revealed that further diagnostic stewardship might be warranted and safe. Here, we also mention three other publications that reported on related findings regarding the shortage of blood culture bottles.1-3
S. aureus bloodstream infections are associated with up to 40% mortality, but standardized management, including obtaining multiple blood cultures, can reduce that mortality by nearly half.1 Investigators at Vanderbilt reviewed the outcomes of patients with S. aureus bacteremia when they reduced the numbers of initial and repeat blood cultures because of the blood culture bottle shortage.1 Although neither the median number of days to clearance of bacteremia nor the duration of intravenous antimicrobial treatment was different before and during the time of restrictions, both the time to diagnosis of community-acquired cases and the rate of clearance within 24 hours were changed by the restrictions.1 With only 187 patients included in the study, the rate of readmissions within 30 days was not significantly different with (30%) and without (21%) blood culture restrictions, but the authors wondered if those data might represent a signal of potential harm to some patients.1 Overall, the Vanderbilt team supported diagnostic stewardship but saw potential for adverse clinical outcomes with reduction of blood cultures for the sub-population of patients who had S. aureus bacteremia.1
The lack of adequate quantities of blood culture bottles also affected adolescent and adult care in Japan.2 There, clinicians ordered fewer sets of multiple cultures and deferred any culture testing in some patients; rates of culture positivity increased.2 Ordering practices returned to or toward baseline when restrictions ended.2 The authors of this report speculated that the increased rate of positive cultures might have been because some of the selective restrictions in culturing reduced some unnecessary testing.2
Staff at a pediatric (non-cardiac) intensive care unit in Colorado used machine learning to develop and validate restrictions in blood culture ordering for use during any future supply chain disruption.3 Clinical data including vital signs, exam findings, and laboratory test results were evaluated as potential predictive factors, and negative predictive value was taken as the primary outcome measure.3 The model (incorporating 20 key factors that mostly related to vital signs and basic laboratory test results) accurately predicted more than 25% of negative blood cultures. Using their algorithm to restrict low-risk sampling, 151 negative cultures could have been avoided for every missed positive culture.3 Of note, each of the “false-negative” predictions during their validation study was actually of a positive culture result later deemed to have been a contaminant.3
Lessons learned during the shortage of blood culture bottles potentially could lead to some improvements in diagnostic stewardship. But changes in indications for blood cultures should be made very carefully, especially when S. aureus is involved.
Philip R. Fischer, MD, DTM&H, is Professor of Pediatrics, Department of Pediatric and Adolescent Medicine, Mayo Clinic, Rochester, MN.
References
1. Humphries RM, Banerjee R, Dupont WD, et al. Association between blood culture bottle shortage and ordering restrictions and clinical outcomes for patients with Staphylococcus aureus bacteremia. Open Forum Infect Dis. 2025;12(9):ofaf546.
2. Ono D, Mimura K, Watanabe Y. Short supply-driven modifications to blood culture practice and their clinical impact: A single-center time-series study. Cureus. 2025;17(7):e88508.
3. Martin B, DeWitt PE, Payan M, et al. Diagnostic stewardship of blood cultures in the pediatric ICU using machine learning. Hosp Pediatr. 2025;15(6):e240-e244.