
Wrist and Finger Dislocations
July 15, 2025
By Simranjit S. Gill, DO; Derrick Huang, DO; and Nicholas Haynie, DO
Injuries to the wrist and fingers, although frequently overshadowed in polytrauma care, demand precise assessment and timely intervention to prevent long-term functional impairment. In this issue, the authors provide a thorough and clinically focused review of these often-complex dislocations, emphasizing both anatomical understanding and evidence-based management strategies relevant to emergency medicine providers. This article offers practical guidance on procedural sedation, diagnostic tools, and injury scoring systems to aid in early recognition and effective treatment. We trust this comprehensive review will serve as a valuable refresher for clinicians aiming to improve patient outcomes through meticulous evaluation and intervention.
— Daniel Migliaccio, MD, Editor
EXECUTIVE SUMMARY
- Hand and finger injuries, while rarely life-threatening, can cause severe functional impairment, making early identification, stabilization, and referral critical to avoid long-term disability.
- Functional outcomes can be poor in polytrauma patients, especially with carpal and metacarpal injuries, which often are underdiagnosed because of the focus on more life-threatening injuries.
- Traumatic hand injuries are associated with high economic burden, particularly in working-age adults, leading to significant time off work (median of 70 days) and are among the costliest injury types globally.
- Hand anatomy includes 27 bones (carpal, metacarpal, and phalanges) with complex joint and ligament structures crucial to mobility; injury mechanisms often affect these components differently depending on direction and force.
- Dislocations of the interphalangeal (IP) joints (distal interphalangeal [DIP], proximal interphalangeal [PIP], metacarpophalangeal [MCP]) are common and named by the direction of the distal bone, with dorsal PIP dislocations being most frequent because of hyperextension.
- Post-reduction evaluation is critical, especially for central slip integrity in volar PIP dislocations, since missed injuries can result in deformities such as pseudo-boutonnière.
- Metacarpophalangeal dislocations, particularly dorsal ones, are common in the index finger and require careful reduction to avoid volar plate entrapment; complex cases may need open reduction.
- High-energy wrist injuries (e.g., perilunate and lunate dislocations, radiocarpal dislocations) are rare but serious, often requiring advanced imaging and surgical intervention, with potential complications like nerve damage and arthritis.
- Sedation and analgesia are vital for successful reduction in the emergency department, with agents like propofol, ketamine, etomidate, and fentanyl used based on patient risk, American Society of Anesthesiologists class, and injury severity.
- The use of proper scoring systems (e.g., Patient-Rated Wrist/Hand Evaluation [PRWE], Quick Disability of Arm, Shoulder, and Hand [QDASH]) may guide functional assessment and follow-up needs.
Introduction
Wrist and finger dislocations, although often overshadowed in polytrauma settings, require prompt recognition and management to prevent permanent dysfunction. Injuries to the hand and fingers are commonly some of the most distressing complaints seen in the emergency department, given the hands’ essential role in daily activities. While these injuries often are non-life-threatening, changes to a patient’s ability to use their hands can be debilitating and distressing. It is the role of the emergency staff to correctly identify, stabilize, prevent further injury, and direct toward definitive treatment that can help prevent lasting disability or worsening outcomes in these types of injuries. This review offers emergency physicians a targeted refresher on relevant anatomy, common dislocation types, and associated complications. It also covers essential diagnostic tools, injury scoring systems, and procedural sedation techniques for safe and effective reduction. While specialist consultation frequently is necessary, early and appropriate emergency care can significantly influence long-term functional outcomes.
Epidemiology
Based on a study using the National Electronic Injury Surveillance System, the incidence rates of finger, hand, and wrist injuries were 450, 264, and 182 per 100,000 people, respectively.1 Overall, 649,131 cases of hand and wrist injuries were identified from 2009 to 2018, estimated to be 25,666,596 patients nationally. According to the National Center for Health Statistics in 2016, 42.3 million emergency department encounters were injury-related, and 26% of those injury-related encounters involved the upper extremity and hand. While these types of injuries have been noted to be in decline over the past decade, there still is a significant percentage of these injuries that present to the emergency department. Considering that most occupations and activities of daily life involve the use of hands and arms, these injuries can be burdensome to patients’ lives. Often, in the setting of polytrauma patients, these injuries go undiagnosed because life-threatening injuries require more immediate attention or intervention, leading to delayed healing or longer-lasting issues.2
A Dutch study collected data from January 2009 to December 2014 in polytrauma patients aged 18 years and older, assessing functional outcome and patient-reported outcomes. Researchers used scoring systems, including the Quick Disability of Arm, Shoulder, and Hand questionnaire (QDASH) and the Patient-Rated Wrist/Hand Evaluation (PRWHE), (both discussed later) to determine patient ranking of disability and lasting pain. Out of 2,046 polytrauma patients, 81% of patients were able to complete the questionnaire with a median 54-month follow-up, and 3.5% of these patients also experienced injuries distal to the radius. They noted that their injuries in the hands were well below the aforementioned expected average. However, out of this group, the researchers found that the metacarpal and carpal regions were the most frequently affected. Patients in their study who had carpal fractures, dislocations, and injuries in multiple regions of the hand had the worst long-term outcomes.2
Although hand and wrist injuries accounted for only 26% of injury-related emergency department visits, they were the most expensive injury type in 2007, according to the Dutch Injury Surveillance System.3 Their estimated costs reached approximately $740 million (USD), surpassing those of knee injuries, lower limb fractures, hip fractures, and even skull-brain injuries.3 Most of this cost is due to productivity costs within the age groups of 20- to 64-year-olds, since they have delays in getting back to work.3
A Korean study in 2023 analyzing the frequency of worker injuries by affected body parts and their associated costs found that hand, wrist, and finger injuries were the most reported single-injury types that affected work. The costs associated with these single-type injuries were only surpassed by multiple-type injuries.4 Another study published in 2018 found that those patients with traumatic hand injuries had a mean of 83 days and a median of 70 days off work.5 This was directly correlated to the type of work and skills needed at work. These types of injuries directly affect those who are considered blue-collar workers more directly.5
Hand Anatomy, Function, and Evaluation
Anatomically, the hand is divided into three different areas: carpus, metacarpus, and phalanges. The carpus has eight bones held tightly by ligaments, arranged in two rows of four. The proximal row from thumb to fifth digit consists of the scaphoid, lunate, triquetrum, and pisiform. In the same direction, the second row consists of hamate, capitate, trapezoid, and trapezium. The first row of the carpus articulates with the distal radius and ulna, forming the radiocarpal joint and ulnar-meniscus-triquetral joint. There are a total of 14 phalanges, with three phalanges each from the second to the fifth digit, and two phalanges in the first digit. Phalanges are named based on their relative positions. Apart from the first digit, which only has proximal and distal phalanges, the second to fifth digits each have proximal, middle, and distal phalanges. Joining the phalanges and carpus, there are five metacarpals. Combining the three areas, there are a total of 27 bones in each hand.6 (See Figure 1.)
Figure 1. Bones of the Hand |
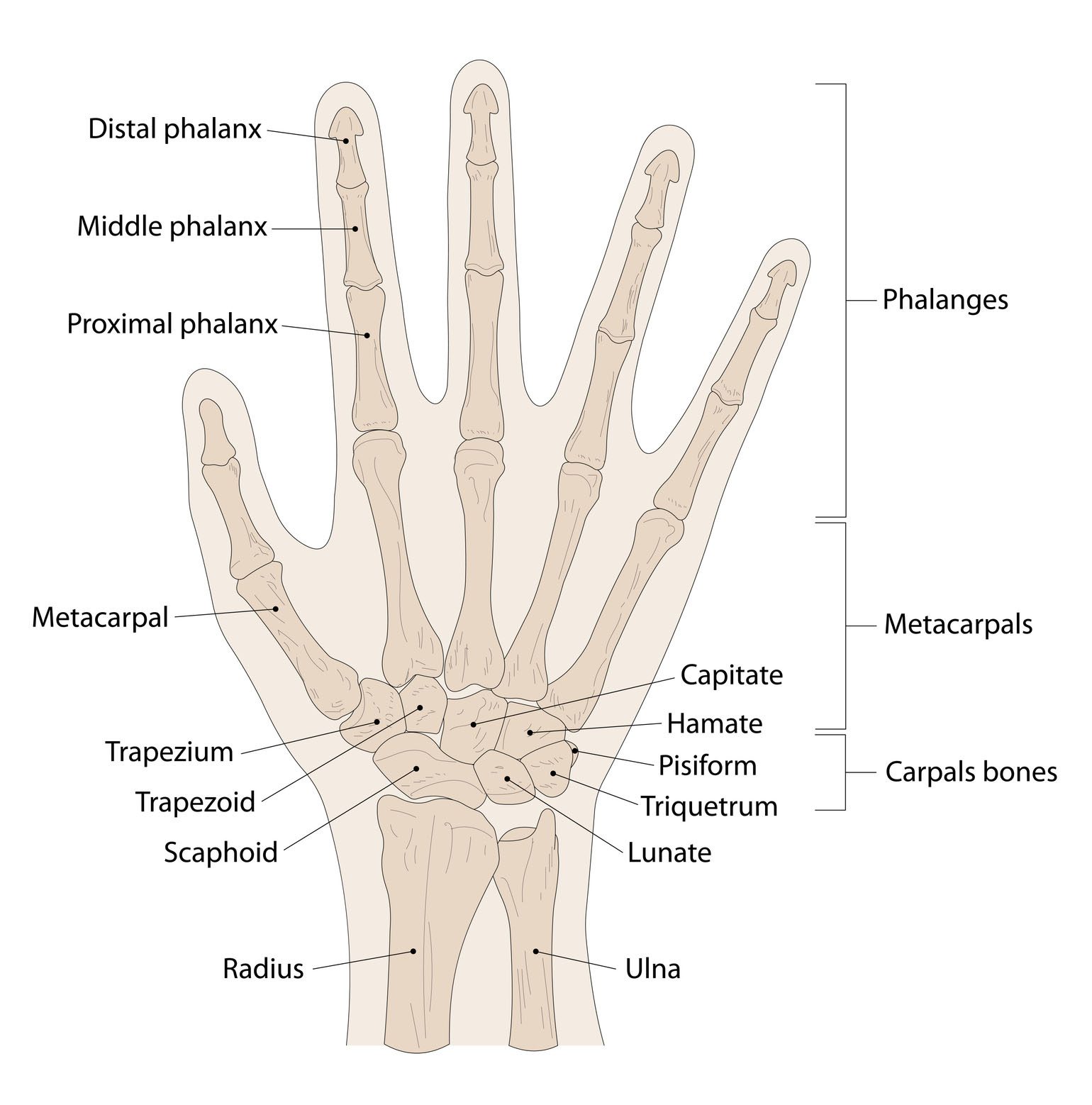 |
Source: Getty Images |
The radiocarpal joint connects the proximal carpal row with the radius and articular disc, while the midcarpal joint lies between the proximal and distal carpal rows, functioning as a compound articulation. These joints enable wrist flexion, extension, radial deviation, and ulnar deviation. The carpometacarpal (CMC) joint, involving the distal carpal row and metacarpal bases (2-5), allows slight gliding movement, with increasing mobility toward the fifth metacarpal, facilitating palm cupping. The trapezio-metacarpal joint is a saddle-shaped articulation between the trapezium and first metacarpal, allowing extensive mobility and often called the “key” joint of the hand. It enables flexion, extension, abduction, adduction, and complex movements like opposition and circumduction. The ulno-menisco-triquetral joint is a “clinical joint” without a synovial cavity, but it aids in supination and pronation through gliding. These joints contribute to wrist and hand movements through traction, gliding, and rotary forces.6 Normal range of motion of the wrist and fingers is found in Tables 1 and 2.
Table 1. Average Wrist or Carpal Range of Motion | |
Average maximum range of motion of the wrist | |
Flexion | 80 degrees |
Extension | 70 degrees |
Ulnar deviation | 30 degrees |
Radial deviation | 20 degrees |
Forearm supination | 80 degrees |
Forearm pronation | 80 degrees |
Adapted from: American Academy of Orthopaedic Surgeons. Joint Motion: Method of Measuring and Recording. American Academy of Orthopaedic Surgeons;1965. Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. 5th ed. F.A. Davis Company;2017. | |
Table 2. Average Range of Motion of Adult Joints in the Digits |
Thumb
Index Finger
Middle Finger
Ring Finger
Little Finger
|
Adapted from: Ngeo JG, Tamei T, Shibata T. Continuous and simultaneous estimation of finger kinematics using inputs from an EMG-to-muscle activation model. J Neuroeng Rehabil. 2014;11:122. |
Ligaments
Most carpal ligaments can be difficult to differentiate, and a discussion of all the ligaments within the hand and wrist is out of the scope of this article. However, it is important to recognize that several key ligaments play a crucial role in the mechanism and stability of dislocation injuries. When evaluating interphalangeal dislocations, it is important to assess both the severity and the direction of the dislocation, since these factors guide management and predict potential complications. For example, distal interphalangeal and proximal interphalangeal dislocations can involve injuries to the collateral ligaments. These ligaments, whether partial or complete ruptures of the collateral ligaments, can directly affect the healing and long-term outcomes after reduction. The proximal interphalangeal joint has a unique structure called the volar plate. This volar plate is a fibrous structure located over the proximal interphalangeal (PIP) joint. Its dense collagen fibers help prevent hyperextension injury.8 This structure can present as a barrier to closed reduction in the emergency setting.
Specific Injuries
Finger Dislocations
Finger dislocations can be described based on the site and direction of the dislocation. Dislocation can happen at the interphalangeal and metacarpophalangeal junctions. Interphalangeal dislocations then can be further classified into proximal and phalangeal dislocations. Generally, the direction of the dislocation is named based on the direction of the distal bone in relation to the proximal bone. For finger or interphalangeal dislocations, these are described as dorsal, volar, and lateral.9 The following sections will present these injuries in order from distal to proximal, since their complexity typically increases in that direction.
Interphalangeal Dislocation
Interphalangeal dislocation can occur at all three joint spaces: distal interphalangeal (DIP), metacarpophalangeal (MCP), and PIP joints.10 These joints are stabilized by collateral ligaments on both the lateral and medial surfaces, preventing most deviation from either direction. Stabilization is provided by both extrinsic and intrinsic tendons and muscles, as well as by key structures such as the central slip and lateral bands. Displacement of the joint surfaces in the phalanges is classified and named based on the distal injury direction. Dislocations may occur in the dorsal, volar, or lateral planes.
PIP dislocation usually happens dorsally from longitudinal compression and hyperextension, such as being hit by a ball at the fingertips, and, thus, dislocation is most likely to happen at the middle finger.11 (See Figure 2.) Volar dislocation is infrequent and has a higher complication rate, with a lower success rate of reduction.12,13 In cases of volar dislocation, the central slip may be ruptured. If left untreated, this can result in a pseudo-boutonnière deformity, characterized by persistent PIP joint flexion with loss of DIP extension.14
Dorsal dislocations most commonly involve hyperextension mechanisms. For simple dorsal PIP and DIP dislocation, the practitioner should apply slight traction to the phalanges on either side of the dislocation and apply extension to realign the articular surfaces. Volar pressure to the proximal base of the distal phalanx often is needed during extension to align the articular surfaces. Pressure is applied until the displaced digit is seated back into anatomical alignment.9
Figure 2. Finger Dislocation of Proximal Interphalangeal Joint |
 |
Source: Hellerhoff. https://commons.wikimedia.org/wiki/File:Finger_luxation_D4_PIP.png |
After reduction, the examiner should evaluate the joint for instability in all planes and obtain radiographs. Closed reduction followed by splinting in slight flexion is used to prevent redislocation and promote healing of the volar plate.10 Both DIP and PIP joint dislocations often are stable after reduction and then are stabilized for orthopedic follow-up by dorsal splinting at 30 degrees of flexion.9
Volar dislocations are less common and usually occur from direct injury to the dorsum of the finger. The reduction occurs similarly to dorsal dislocations. Gentle traction is applied to the surrounding phalanges; however, gentle flexion and dorsal pressure to the proximal base of the distal phalanx is applied to approximate the articular surfaces. These closed reductions typically are successful with closed techniques. Post-reduction splinting in full extension for four to six weeks will allow the dorsal structures to heal.10
Of note, post-reduction testing of the central slip should be performed after volar PIP dislocations. This is performed post-reduction by placing the affected joint over a 90-degree corner of a surface in 90 degrees of flexion. The patient is instructed to extend the affected finger against resistance. If the patient is unable to extend the PIP, then there is an assumption of some central slip ligament damage from the volar injury. Often, the DIP will still be able to extend with central slip injuries.10
Lateral dislocations typically are from lateral- or medial-type forces to the distal phalanx. Closed reduction is performed similarly to the those previously mentioned, with gentle traction and opposing pressure to the proximal portion of the distal phalanx. Often, more traction is needed in these dislocations because of the lack of flexion or extension able to help realign the articular surfaces. Often, disruption of the collateral ligaments is present. If closed reduction is successful, “buddy taping” to the adjacent finger for stability generally is well tolerated.10
In general, interphalangeal dislocation complications include joint stiffness, chronic instability, and post-traumatic arthritis.15 Unsuccessful closed reductions may require open reduction, which is more common if there are surrounding fractures or soft tissue impingement complicating the closed reduction.16 All dislocations with attempts, whether successful or not, require orthopedic follow-up.9 Prevention of joint stiffness involves early referral to occupational therapy, where guided active range of motion exercises can aid in functional recovery.
Metacarpophalangeal Dislocation
Dorsal MCP dislocations are most commonly encountered in the index and sometimes small fingers, typically from forced hyperextension of the digit on an outstretched hand. These present as obvious deformities and require imaging to assess the extent of injury or the presence of osseous injury. One key structure that helps prevent dislocation is the volar plate, a dense fibrocartilaginous component of the joint capsule located on the palmar aspect of the joint. Its primary function is to resist hyperextension. As a result, most interphalangeal dislocations occur dorsally rather than laterally or volarly. (See Figure 3.)
Figure 3. Joint Dislocation of the Metacarpophalangeal Joint |
 |
Source: Hellerhoff. Wikimedia commons. https://commons.wikimedia.org/wiki/File:Finger_luxation_D5_MCP.png |
In a simple dislocation, the volar plate remains in place over the metacarpal.10 In the case of complex dislocation, the volar plate and other structures like the palmar plate, flexor tendons, and lumbrical muscles can become entrapped.17,18 The lumbrical muscles consist of four intrinsic muscles of the hand that are located in the palm. They originate from the flexor digitorum profundus and insert onto the lateral bands of the extensor tendons. The first and second lumbricals are innervated by the median nerve, and the third and fourth lumbricals are innervated by the ulnar nerve. These provide flexion for the metacarpophalangeal joints. Along with volar plate injuries, these muscles can become trapped or torn with dislocation injuries of the metacarpophalangeal joints.19
The lateral view X-ray will be the best to evaluate for dislocation; anteroposterior (AP) and oblique views also should be obtained. Careful assessment of the joint space is essential, since any widening may indicate the presence of a complex dislocation. American College of Radiology guidelines recommend that a three-view (AP, lateral, and oblique views) generally is sufficient for most finger injuries.20 According to these guidelines, soft tissue injuries are best evaluated with magnetic resonance imaging (MRI). There is minimal to no role of computed tomography (CT) scans for soft tissue injuries of the hand and fingers. MRI provides the best surgical planning for the future. MRI may be used to assess capsule and collateral ligament injuries of the PIP and MCP joints.20 Typically, these MRIs are performed on an outpatient basis and not in the emergency department.
Lateral dislocation is likely when ulnar or radial deviation is observed. These types of dislocations often injure the collateral ligaments that provide MCP joint stabilization.21 Closed reduction of these injuries includes realignment of the joints and “buddy taping” for support. The most common MCP joints to experience lateral dislocations include the index finger and fifth finger because of a lack of supporting structures on both sides.
Volar dislocation occurs from hyperflexion or hyperextension of the joint. Simple dislocations usually can be managed with a closed reduction technique, while complex dislocation often requires open reduction.22
For a dorsal dislocation, flex the wrist to reduce tension on the intrinsic and extrinsic flexors, then apply direct pressure over the dorsal aspect of the proximal phalanx. Avoid longitudinal traction to prevent entrapment of the volar plate. The patient should receive a dorsal blocking splint to maintain reduction and support healing and should have close follow-up with a hand surgeon.
For a volar dislocation, flex the MCP, then apply direct pressure over the volar aspect of the proximal phalanx. This injury pattern should be immobilized in 30 degrees of flexion for two weeks, at which point it may be switched to a dorsal blocking splint by a subspecialist. Complications of MCP dislocations include joint stiffness, arthritis, osteonecrosis of the metacarpal head, and premature closure of the physis in certain populations.21
Specific Deformities
Not all deformities of the fingers are dislocations. Most polytrauma or even single injuries to the hands are related to fractures or other complex injuries. There are even some chronic arthritis-type deformities that can be severe enough to look as if there are subluxed joints that need to be addressed. Swan neck deformity is seen as hyperextension of the PIP joint and flexion of the DIP joint. It can arise from volar MCP subluxation, laxity of the PIP volar plate, flexor digitorum superficialis laceration, contractures, or mallet fingers. Boutonnière deformity typically is seen with PIP injuries involving the central slip. Without appropriate central slip mechanisms, extension of the affected finger results in a pathological flexion with the lateral bands still acting on the DIP to cause extension.23
Both deformities are managed with corrective splinting with hand orthopedic follow-up for possible surgical intervention to include tenodesis or central slip tenotomy.24
Wrist Dislocation
Perilunate Dislocation
Because of the high energy associated with these injuries, perilunate dislocations, lunate dislocations, and perilunate fracture-dislocations account for less than 10% of all wrist injuries.25 High force applied to a hyperextended wrist in situations such as falls from heights on an outstretched hand or motor vehicle collisions can destabilize the surrounding structure through fractures and disruptions in articulations or ligaments, which may cause a perilunate dislocation, lunate dislocation, and/or perilunate fracture-dislocation. (See Figure 4.) The mechanism typically is wrist hyperextension, ulnar deviation, and intercarpal supination. In the case of perilunate dislocation, the lunate maintains its articulated position with the distal radius while the surrounding carpal bones dislocate dorsally. The most common symptoms are pain, swelling, and deformity. Loss of grip strength can occur, as well as median nerve compression, leading to paresthesia or numbness in the median distribution.26,27 This typically is present with more instability than lunate dislocations because of the involvement of multiple carpal bones.
Figure 4. Perilunate Fracture Dislocation |
 |
Source: Hellerhoff. https://commons.wikimedia.org/wiki/File:Transscaphoid_perilunate_fracture-dislocation_-_39jm_-_Roe_ap_und_seitlich_-_001.jpg |
The Mayfield classification divides perilunate instability into four stages. In stage one, there is rotatory subluxation of the scaphoid, disrupting the scapholunate ligament. On AP X-ray, increased distance indicates scapholunate dissociation for more than 3 mm can be seen, known as the Terry-Thomas sign. Stage two involves the lunocapitate disruption, and the lunate can project through the space of Poirier, which is an area between the capitate and lunate that has poor ligamentous support. In this stage, the lunate remains within normal alignment with the distal radius, where the remaining carpal bones are dislocated. Scaphoid fractures are common and typically are present in up to 60% of cases of lunocapitate disruption. In stage three, the lunotriquetral interosseous ligament is disrupted. Triquetral fracture also can be seen with this stage of injury. In this stage, neither the lunate nor capitate is aligned with the distal radius. The lunate is dislocated in stage four, involving the dorsal radiolunate ligament. A tipped teacup appearance can be seen on X-ray. (See Figure 5.) Physicians can attempt closed reduction, but it often is unsuccessful because of the complexity.26,27 Open reduction and internal fixation (ORIF) is the gold standard in treatment for this type of injury and allows for repair of ligamentous and bony injuries.26,27
Figure 5. Lunate Dislocation with Spilled Teacup Sign |
 |
Source: James Heilman, MD. https://commons.wikimedia.org/wiki/File:LunatedislocationL.jpg |
Perilunate dislocations typically are caused by high-energy traumas, such as falls from heights or motor vehicle collisions. The mechanisms typically involve wrist hyperextension, ulnar deviation, and intercarpal supination. The force vector travels from radial to ulnar direction, causing instability and damage to the complex ligamentous structures of the wrist. The most common symptoms are pain, swelling, and deformity. Loss of grip strength can occur, as well as median nerve compression, leading to paresthesia or numbness in the median distribution.26,27 Perilunate dislocations typically present with more instability than lunate dislocations because of the involvement of multiple carpal bones. Hand radiography usually is sufficient for diagnosis; however, CT scanning can be useful in assessing the extent and surgical planning.27
Unfortunately, perilunate dislocations have a higher risk of complex regional pain syndrome, median nerve dysfunction, and tendon issues. There also is the risk of developing post-operative arthritis if operative intervention is required.26
Lunate Dislocation
Lunate dislocations also occur from high-energy traumas such as falls from a height or motor vehicle accidents. The mechanisms are similar to those of perilunate dislocations, except lunate dislocations typically have volar displacement from their anatomical location. The type of movement that typically causes a lunate dislocation is forced hyperextension of the wrist, often combined with ulnar deviation and intercarpal supination. The force vector travels from radial to ulnar direction, causing instability and damage to the complex ligamentous structures of the wrist. Lunate dislocation symptoms and treatment options are similar to perilunate dislocation symptoms, as mentioned earlier.25,26 (See Figure 5.)
Even with appropriate operative reduction post-injury, long-term follow-up is required for post-operative arthritis. Because of the location and anatomy, median nerve dysfunction and even avascular necrosis of the lunate are possible complications from lunate dislocations.27
In patients with perilunate and/or lunate dislocations, the provider should obtain consultation for disposition planning and to ensure appropriate management and optimal functional recovery.
Radiocarpal Dislocation
Radiocarpal dislocation is a rare, severe wrist injury that only accounts for 0.2% resulting from high-energy trauma, such as falls from height, motor vehicle collisions, etc.28 Radiocarpal dislocation is a complex injury and can be associated with bone injuries, nerve injury, or beyond loss of contact between the carpus and the radius, extending into carpal bone fracture or intercarpal injuries.29 In comparison, distal radius fractures, such as shearing or rotation fractures, can be intra-articular, but the radius remains in contact with the carpus. The mechanism involves severe shear or rotation force to a hyperextended and pronated wrist. Radiocarpal dislocations often present with concomitant osseous injury.13 Both the distal radius and ulna can have associated fractures.30 The medial and ulnar nerves both can be involved, with the medial nerve more commonly involved than the ulnar; both can lead to numbness or weakness in the hand. Like other finger and wrist dislocations, radiocarpal dislocation can happen both dorsally and ventrally. Dorsal dislocation is much more common than ventral dislocation.
Different classifications have been proposed. Moneim’s classification of radiocarpal dislocations distinguishes between two types. Type I involves a radiocarpal dislocation without associated ligamentous injury, while type II includes both a ligamentous injury and a radiocarpal fracture-dislocation, often with an associated fracture of the radial or ulnar styloid.31 The short radiolunate ligament attaches to the volar lunate facet of the distal radius, restraining against volar translation of the carpus. The radioscaphocapitate ligament attaches to the radial styloid to help prevent ulnar translation of the carpus. Dumontier’s classification is based on the severity of the fracture of the radial styloid process. Type II is defined by fracture of more than one-third of the width of the scaphoid fossa, and all other dislocations are classified into type I.31
Symptoms associated with radiocarpal dislocations can include pain, swelling, and deformity to the hand. Although neurological complications (such as median nerve compression) are more frequently reported, vascular compromise (such as diminished pulses or capillary refill) can occur as a result of displacement of carpal bones, swelling, or direct vessel injury.13 Physical examination combined with radiographic X-ray usually is sufficient to identify this type of injury as well as associated fractures. If neurovascular injury is suspected, an urgent closed reduction attempt is warranted. This is difficult and often is unsuccessful because of the complexity of these injuries.13 The majority of these injuries require orthopedic intervention through ORIF.
Complications from these high-energy injuries include ulnar translation of the carpal bone leading to multidirectional instability, loss of motion, post-traumatic arthritis, osteoarthritis, and secondary wrist fusion.32
Sedation Methods
If attempts at reduction are started in the emergency department, adequate sedation or analgesia greatly improves reduction techniques. If the patient is able to tolerate it, analgesia alone could be an option for those requiring a simple reduction. For those with interphalangeal dislocations or injuries, one could attempt digital nerve block if prolonged reduction or manipulation is expected.33
Levels of sedation are determined by responsiveness and ability to maintain airway, breathing, and circulation. Fractures and dislocations often cause significant pain and may necessitate the use of deep sedation. Deep sedation is defined by a markedly depressed level of consciousness in which the patient retains the ability to respond purposefully to repeated or painful stimuli.32 Choosing a level of sedation should be well thought out and discussed before any procedure with the patient. The risks and benefits of sedation methods need to be considered.
A patient’s airway potentially can be impaired while the patient is in a deep sedation state, while it usually is maintained in dissociative and moderate sedation. In minimal sedation, the airway is unaffected. Cardiovascular function usually is unaffected in minimal to deep sedation; however, it can be impaired in patients receiving general anesthesia (the patient is not arousable, even by painful stimulation). However, it is important to note that different agents used in sedation may have effects on blood pressure.32
Responsiveness is another key component when assessing a patient’s level of sedation. It ranges from normal but slowed response to verbal stimulation in minimal sedation to not arousable in general anesthesia. Patients in deep sedation require noxious stimuli to elicit a response. In a dissociative state, patients can be in a trance-like state and have variable responsiveness. Patients in a moderate sedation state may require some physical stimulation, but they often can respond to verbal stimulation as well.32
The American Society of Anesthesiologists (ASA) physical status classification system was designed to help anesthesiologists determine the risk for general anesthesia; however, it can help emergency physicians classify patients’ risk for procedural sedation. The details of this classification system are not discussed here, but generally, the lower the class, the lower the chance of significant complications. In classes one and two, the significant risk is less than 5%.34
Common complications or adverse events from sedation in the emergency department include agitation, apnea, aspiration, bradycardia, hypotension, hypoxia, intubation, laryngospasm, and vomiting.35
Agent Selection
Commonly used sedation agents include propofol, ketamine, fentanyl, etomidate, and midazolam.
Propofol has a rapid onset and a short duration. Sedation occurs within 30 to 60 seconds after injection and only lasts about five to six minutes. Propofol has multiple effects, including muscle relaxation, sedation, and amnesia. Importantly, propofol does not have analgesic properties. The most serious adverse effects of propofol are rapidly developing respiratory depression, apnea, and hypotension. Propofol produces hypotension through negative inotropy and vasodilation, and it is more common in hypovolemic patients and high ASA physical status. Prior to providing sedation, it is important that hypovolemia is corrected and that ventilatory support equipment is available nearby before sedation. The recommended dose is 0.5 mg/kg to 1.0 mg/kg intravenous (IV), followed by 0.5 mg/kg every three minutes if needed. For the older adult patient, sedation may need to be cut in half to decrease complications.36
Unlike other procedural sedation agents, ketamine possesses both analgesic and anxiolytic properties. Ketamine produces a state of dissociation, characterized by profound analgesia, sedation, and amnesia. Ketamine acts on multiple pathways through dopamine, norepinephrine, serotonin, and opioid receptor antagonism that can cause psychotropic effects, including hallucination, synesthesia, pronounced derealization, and depersonalization. Dissociative state does not usually appear until 1 mg/kg to 1.5 mg/kg IV or 3 mg/kg to 4 mg/kg intramuscular (IM). Unlike propofol, ketamine has minimal depressant effects on blood pressure and usually preserves ventilator effort. Hypersalivation and bronchorrhea had been reported with ketamine. If observed, atropine and glycopyrrolate can be provided. Previously, the use of ketamine in the emergent setting has been limited because of increased intracranial pressure in animal studies. However, in a prospective study, ketamine has not been found to increase intracranial pressure.36
The combination of ketamine and propofol, known as ketofol, can promote hemodynamic stability and result in fewer respiratory adverse events compared to propofol alone. The combination prolongs the duration of sedation compared to propofol by itself.36
Because of its rapid onset and short duration of action, etomidate often is used for rapid sequence intubation in the emergency department. It also may be used as an agent for procedural sedation. The procedure dose for etomidate is 0.1 mg/kg to 0.2 mg/kg, with an optional repeat dose of 0.05 mg/kg every three to five minutes. The onset is less than one minute, and it lasts four to 15 minutes. Compared to propofol, etomidate has similar respiratory adverse events and less effect on hemodynamic stability, but more myoclonus. Because of its shorter action, etomidate is better for cardioversions and is less useful for longer procedures, such as reductions.36
Fentanyl often is used for analgesia for sedation in the emergency department. Fentanyl dosing usually is 0.5 mcg/kg to 1.5 mcg/kg in most patients and lowered to 0.25 mcg/kg in older adult patients. It can be repeated every one to three minutes. Although fentanyl typically is not associated with respiratory depression and hypotension when used alone, the incidence goes up when used in combination with sedatives.36
Benzodiazepines, such as midazolam, have amnestic, anxiolytic, and sedative properties. Midazolam often is used in combination with ketamine and fentanyl. Dosing of midazolam is 1 mg to 2.5 mg given as a slow IV push; weight-based dosing is 0.1 mg/kg, but larger doses can be associated with more adverse effects.36
Injury Scoring Systems
As discussed earlier, multiple scoring systems have been developed to determine long-term outcomes and help evaluate finger and wrist injury types.
PRWE/PRWHE is a 15-item rating questionnaire and an optional aesthetics question designed to measure wrist pain and disability in the activities of daily living. Patients can rate their pain and disability from 0 to 10. The scale has five subscale questions on pain, rating pain while at rest, when doing repeated wrist movement, when lifting a heavy object, when it is at its worst, and how often patients experience pain. Functional portions of the questionnaire are split into specific activities and usual activities. Specific activities include turning a doorknob, cutting meat using a knife, fastening buttons, pushing up from a chair, carrying one 10-pound object, and using bathroom tissue. In usual activities, patients will rate on personal care activities, household work, work activities, and recreational activities. The final question asks the patient to rate their wrist/hand today as a percentage of normal (0% to 100%), with 100% being normal.37
Another scoring system is the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire, designed to evaluate the degree of difficulty a patient experiences in performing various physical activities. Quick DASH (QDASH) is an abbreviated version that only contains 11 items measuring a patient’s ability to complete tasks and absorb forces, and the severity of symptoms. QDASH uses a five-point Likert scale for patients with one or more upper extremity musculoskeletal disorders. Questions 1-6 ask patients to rate their ability to open a tight or new jar, perform heavy household chores, carry a shopping bag or briefcase, wash their back, use a knife to cut food, and participate in recreational activities. Questions 7 and 8 ask about a patient’s ability for social activities, and work or other regular daily activities, respectively. Questions 9 and 10 ask for symptoms, including pain and tingling. The last question is about how pain in their upper extremities affects their sleep. There also are two optional sections for work modules, sports, and performing arts modules.38,39
Conclusion
Injuries related to the finger and wrist are common in the emergency department. Although most wrist and finger injuries typically are not life-threatening, if not accurately diagnosed and treated in the emergency department, they can lead to complications, most commonly stiffness, limited range of motion, instability, numbness and tingling if there is nerve involvement, and delayed healing.40 The evaluation of a patient presenting with finger and wrist injuries includes a thorough examination of the patient’s neurovascular and functional status. Most of the dislocations can be evaluated using plain film, but in some cases, MRI is warranted for complex fractures that might involve ligaments or tendons, or it may be used in difficult-to-reduce dislocations.41 CT sometimes is used for better evaluation of bone, especially in lunate dislocation associated with fracture.41
Closed reduction may be attempted most of the time in the emergency department, and depending on the injury, the patient can be discharged with orthopedic follow-up. Those patients with complex injuries or who have a dislocation that is unable to be reduced in the emergency department might require specialist consultation and/or open reduction in the operating room. The sedation strategy will depend on the patient’s past medical history and injury severity.36 Early and appropriate emergency care can significantly influence long-term functional outcomes.
Simranjit S. Gill, DO, is Assistant Professor, Emergency Medicine Clerkship Director, Emergency Medicine, Wright State University, Dayton, OH.
Derrick Huang, DO, is Emergency Medicine Resident, Boonshoft School of Medicine, Wright State University, Dayton, OH.
Nicholas Haynie, DO, is Emergency Medicine Resident, Boonshoft School of Medicine, Wright State University, Dayton, OH.
References
1. Gordon AM, Malik AT, Goyal KS. Trends of hand injuries presenting to US emergency departments: A 10-year national analysis. Am J Emerg Med. 2021;50:466-471.
2. Ferree S, van der Vliet QMJ, van Heijl M, et al. Fractures and dislocations of the hand in polytrauma patients: Incidence, injury pattern and functional outcome. Injury. 2017;48:930-935.
3. de Putter CE, Selles RW, Polinder S, et al. Economic impact of hand and wrist injuries: Health-care costs and productivity costs in a population-based study. J Bone Joint Surg Am. 2012;94(9):e56.
4. Bae SW, Lee MY, Park SW, et al. Frequency and cost of claims by injury type from the Korea workers’ compensation insurance between 2016 and 2019. J Occup Environ Med. 2023;65(5):e306-e311.
5. Eisele A, Dereskewitz C, Kus S, et al. Factors affecting time off work in patients with traumatic hand injuries — A bio-psycho-social perspective. Injury. 2018;49:1822-1829.
6. Wadsworth C. Clinical anatomy and mechanics of the wrist and hand. J Orthop Sports Phys Ther. 1983;4(4):206-216.
7. Ngeo JG, Tamei T, Shibata T. Continuous and simultaneous estimation of finger kinematics using inputs from an EMG-to-muscle activation model. J Neuroeng Rehabil. 2014;11:122.
8. Williams EH, McCarthy E, Bickel KD. The histologic anatomy of the volar plate. J Hand Surg Am. 1998;23(5):805-810.
9. Borchers JR, Best TM. Common finger fractures and dislocations. Am Fam Physician. 2012;85(8):805-810.
10. Childress MA, Olivas J, Crutchfield A. Common finger fractures and dislocations. Am Fam Physician. 2022;105:631-639.
11. Kolovich GP, Heifner JJ. Proximal interphalangeal joint dislocations and fracture-dislocations. J Hand Surg Eur Vol. 2023;48(2_suppl):27S-34S.
12. Prucz RB, Friedrich JB. Finger joint injuries. Clin Sports Med. 2015;34(1):99-116.
13. Ilyas AM, Mudgal CS. Radiocarpal fracture-dislocations. J Am Acad Orthop Surg. 2008;16:647-655.
14. Lo I, Richards RS. Combined central slip and volar plate injuries at the PIP joint. J Hand Surg Br. 1995;20(3):390-391.
15. Kamnerdnakta S, Huetteman HE, Chung KC. Complications of proximal interphalangeal joint injuries: Prevention and treatment. Hand Clin. 2018;34(2):267-288.
16. Elfar J, Mann T. Fracture-dislocations of the proximal interphalangeal joint. J Am Acad Orthop Surg. 2013;21(2):88-98.
17. Patterson RW, Maschke SD, Evans PJ, Lawton JN. Dorsal approach for open reduction of complex metacarpophalangeal joint dislocations. Orthopedics. 2008;31:1099.
18. Afifi AM, Medoro A, Salas C, et al. A cadaver model that investigates irreducible metacarpophalangeal joint dislocation. J Hand Surg Am. 2009;34:1506-1511.
19. Wang K, McGlinn EP, Chung KC. A biomechanical and evolutionary perspective on the function of the lumbrical muscle. J Hand Surg Am. 2014;39:149-155.
20. Expert Panel on Musculoskeletal Imaging; Torabi M, Lenchik L, Beaman FD, et al. ACR Appropriateness Criteria Acute Hand and Wrist Trauma. J Am Coll Radiol. 2019;16:S7-S17.
21. Dinh P, Franklin A, Hutchinson B, et al. Metacarpophalangeal joint dislocation. J Am Acad Orthop Surg. 2009;17:318-324.
22. Beutel BG, Wang J, Taqi M. Finger dislocation. In: StatPearls [Internet]. StatPearls Publishing. Updated June 2, 2025. https://www.ncbi.nlm.nih.gov/books/NBK551508/
23. Hanson ZC, Thompson RG, Andrews JR, Lourie GM. Boutonniere versus pseudoboutonniere deformities: Pathoanatomy, diagnosis, and treatment. J Hand Surg Am. 2023;48:489-497.
24. Elzinga K, Chung KC. Managing swan neck and boutonniere deformities. Clin Plastic Surg. 2019;46(3):329-337.
25. Rachunek-Medved K, Medved F, Besz W, et al. Do perilunate dislocations and fracture-dislocations result in different radiological outcomes following wrist alignment reconstruction? A single-center retrospective study including 51 patients with perilunate injuries. Arch Orthop Trauma Surg. 2025;145(1):106.
26. Stanbury SJ, Elfar JC. Perilunate dislocation and perilunate fracture-dislocation. J Am Acad Orthop Surg. 2011;19:554-562.
27. Goodman AD, Harris AP, Gil JA, et al. Evaluation, management, and outcomes of lunate and perilunate dislocations. Orthopedics. 2019;42:e1-e6.
28. Pilc E, Washburn S, Tuten HR. Volar radiocarpal dislocation in a child with trisomy 21: A case report. HSS J. 2024;20(2):306-309.
29. Yuan BJ, Dennison DG, Elhassan BT, Kakar S. Outcomes after radiocarpal dislocation: A retrospective review. Hand (N Y). 2015;10(3):367-373.
30. Meena S, Sharma P, Sambharia AK, Dawar A. Fractures of distal radius: An overview. J Family Med Prim Care. 2014;3(4):325-332.
31. de Paula EJL, de Novaes França Bisneto E, Paulos RG, Junior RM. Radiocarpal fracture disloctaions: A new classification and treatment proposal. Acta Ortop Bras. 2022;30(1):e248404.
32. Miner JR, Huber D, Nichols S, Biros M. The effect of the assignment of a pre-sedation target level on procedural sedation using propofol. J Emerg Med. 2007;32(3):249-255.
33. Gottlieb M, Penington A, Schraft E. Digital nerve blocks: A comprehensive review of techniques. J Emerg Med. 2022;63(4):533-540.
34. Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status — historical perspectives and modern developments. Anaesthesia. 2019;74(3):373-379.
35. Bellolio MF, Gilani WI, Barrionuevo P, et al. Incidence of adverse events in adults undergoing procedural sedation in the emergency department: A systematic review and meta-analysis. Acad Emerg Med. 2016;23(2):119-134.
36. Benzoni T, Agarwal A, Cascella M. Procedural sedation. In: StatPearls [Internet]. StatPearls Publishing. Updated March 22, 2025. https://www.ncbi.nlm.nih.gov/books/NBK551685/
37. MacDermid JC. The PRWE/PRWHE update. J Hand Ther. 2019;32:292-294.
38. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: The DASH (Disabilities of the Arm, Shoulder, and Hand). The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602-608.
39. Beaton DE, Katz JN, Fossel AH, et al. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder, and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14:128-146.
40. Kamnerdnakta S, Huetteman HE, Chung KC. Complications of proximal interphalangeal joint injuries: Prevention and treatment. Hand Clin. 2018;34(2):267-288.
41. Hile D, Hile L. The emergent evaluation and treatment of hand injuries. Emerg Med Clin North Am. 2015;33(2):397-408.