
Using Ultrasound in the Care of Pediatric Trauma Patients
September 1, 2025
By Matthew D. Holmes, MD; Lucy Hale, DO; and Titus Chu, MD
Executive Summary
- Trauma is the leading cause of morbidity and mortality in pediatric patients in the United States, with the majority of cases resulting from blunt mechanisms such as motor vehicle accidents. Early diagnosis of life-threatening injuries is critical, and ultrasound has emerged as a valuable point-of-care tool that offers rapid, noninvasive, and radiation-free assessment at the bedside.
- Since its formal integration into trauma protocols in the 1990s, ultrasonography has replaced diagnostic peritoneal lavage in many settings, with the Focused Assessment with Sonography for Trauma (FAST) and Extended FAST (E-FAST) exams serving as central components of pediatric trauma evaluation. While FAST is less sensitive in pediatric populations than in adults, its role in identifying free fluid, especially in the pelvis, is well-supported when anatomical differences and limitations are understood. E-FAST expands diagnostic capability by detecting lung pathology that could require immediate intervention.
- Ultrasound’s utility extends beyond abdominal and thoracic imaging. It enhances vascular access success rates, improves foreign body localization, and allows real-time evaluation of musculoskeletal injuries such as fractures and effusions. Additionally, ultrasound-guided regional anesthesia, such as the fascia iliaca block, provides targeted pain control with improved safety and efficacy in pediatric trauma settings.
- Despite some limitations, particularly in sensitivity compared to computed tomography imaging, ultrasound remains a critical adjunct for pediatric trauma assessment. It combines speed, safety, and diagnostic breadth — qualities essential for managing high-acuity pediatric patients in emergency and prehospital environments.
Introduction
Trauma is the leading cause of morbidity and mortality in pediatric patients in the United States, with most being related to blunt trauma.1 In 2022, more than 15,000 deaths from among people ages 1-19 years were the result of unintentional injury, with the majority being related to motor vehicle accidents.1 Traumatic injuries are time-sensitive, and any amount of delay in injury identification can negatively affect morbidity and mortality.2 Rapid bedside diagnoses can be made with a succinct and specific tool: ultrasonography.
Although ultrasound has a deep history, from its use to detect submarines during World War II to measurement of fetal head diameters, the application to patients who sustained trauma officially began in 1993 and subsequently was standardized in 1997.3,4 Ultrasound has been recognized for its ability to evaluate intraperitoneal injuries at the bedside at a markedly improved speed, with high sensitivity, and in a noninvasive manner when compared to its predecessor, diagnostic peritoneal lavage (DPL).5-7
Pediatric ultrasonography for trauma has been mentioned as early as 1993, with significant studies in the preceding years to establish its role in the younger population.8,9 The Focused Assessment using Sonography for Trauma (FAST) exam has been of particular interest given its contribution to improved outcomes and mitigation of increased oncologic risk.10-13 The extended FAST (EFAST) exam is even more comprehensive because it includes an evaluation of the lungs, for which interpretation can be made to diagnose pneumothoraces, hemothoraces, and effusions.14 This article summarizes these findings as well as presents the basics of ultrasound in pediatric trauma.
Ultrasound Basics
Sound. Sound is a type of mechanical energy that is characterized by wavelength, frequency, and speed. Wavelength is the distance between repeating points on a cycle (millimeters), frequency is the number of times that wave or cycle repeats per second (Hertz, Hz), and speed is the distance traveled per unit of time (meters per second). “Ultra”-sound refers to the high number of times the wave repeats, which is more than 20 kHz; most medical instruments range from 1 MHz to 15 MHz.15
Beam. An ultrasound beam penetrates an object and, based on the impedance of tissues, the sound will be reflected, refracted, scattered, absorbed, or attenuated. Impedance can be thought of as the tissue’s stiffness. If two tissues have similar impedance, then sound will continue to travel, but if there is a large difference in impedance, most will be reflected (bounce back to the transducer) and not travel through the object. Refraction represents a change in the direction of sound when the impedance of two tissues is different and not perpendicular to the direction of the beam. Attenuation is the loss of intensity and amplitude as the sound travels. This can occur through a process called absorption, where the sound is converted into heat as it travels, or through a process called scattering.15
Color. Scattering occurs when the sound bounces off tissues with varying impedance. The intensity of waves returning to the probe are interpreted as brightness. Tissues that reflect more sound waves are brighter, or hyperechoic. Hypoechoic tissue does not reflect as much sound and, thus, appears dimmer. Anechoic tissues return little to no sound and are seen as black. Isoechoic tissues reflect a similar intensity of sound and, therefore, have similar brightness.15
Ultrasound Transducers for Pediatric Trauma
Different probes provide different levels of “clarity” depending on their set frequency, and, thus, different probes are needed for varying clinical questions. In the pediatric patient, the probe used may vary with the age and size of the child.
Phased Array Probe. A smaller footprint probe that creates a triangular beam to penetrate tissue and create a large field of view at depth.16 This does have worse resolution, but it can provide better motion images, such as when evaluating the cardiac window.
Curvilinear Probe. A curved transducer that has a wide footprint that provides better depth but less resolution.¹⁷ This is the most commonly used probe when evaluating the abdomen because it provides the best evaluation of deep organs.
Linear Probe. A linear transducer that uses a rectangular beam to create a high-resolution image at lower depths.17 This is a great option for lung, musculoskeletal, or vascular evaluation in adult-sized children, but it also may be used for cardiac or even abdominal evaluation in neonates and infants. This is the preferred probe for completing bedside procedures, including intravenous access (including central lines) and superficial nerve blocks.
Focused Assessment with Sonography for Trauma
The FAST exam is indicated as an adjunct to the primary survey of Advanced Trauma Life Support (ATLS) when a patient has sustained blunt trauma — this holds true for both the adult and pediatric population.18 In adult populations, the FAST exam has a sensitivity of approximately 42% to 96% and a specificity of 83% to 100% for detecting peritoneal bleeding in blunt trauma.19-22 In the pediatric population, the FAST exam is noted to be lower in both categories, with sensitivity of 27% to 52% and specificity of 91% to 96%, although some newer studies note higher rates of 89% and 99%, respectively.23-27 This advancement may be due to technological improvements or increased availability of training, while the wide variation can be attributed to the anatomic and physiologic differences that will be discussed next.
Right Upper Quadrant
This view is obtained by placing the curvilinear probe with the transducer marker directed cephalad at the anterior axillary line in plane with the patient’s elbow, then moving the probe posteriorly until the liver, kidney, and diaphragm are visualized in long axis. Probe pressure should be minimal to avoid displacing small fluid collections. High-frequency linear probes may be considered for neonates and infants to enhance superficial resolution. Dynamic scanning, or “sweeping,” in both longitudinal and transverse planes, improves sensitivity and ensures the diaphragm, liver edge, and renal capsule are evaluated.
The primary goal is to identify Morison’s pouch, the potential space between the liver and right kidney, and evaluate for the presence of free fluid. Morison’s pouch is the most sensitive site for detecting intraperitoneal fluid in adults, since it is the most dependent area while the patient is supine. However, in pediatric patients this view can be more technically challenging because of a smaller and more anteriorly positioned Morison’s pouch, limited intra-abdominal fat, and greater tissue compressibility that can obscure free fluid accumulation or displace it away from the probe. Additionally, the pediatric liver may cover more of the right kidney than in adults, requiring careful angulation or sweep to fully visualize the space.
In trauma, anechoic fluid collections may be seen between the liver and kidney, along the hepatic edge, or between the liver and abdominal wall. Although Morison’s pouch is the first location where fluid collects in adults, studies suggest that the pelvis is more sensitive in pediatric patients, often revealing free fluid before the right upper quadrant (RUQ) in children with hemoperitoneum.28 In one prospective study of pediatric trauma patients, the pelvis detected fluid in 66% of positive exams compared to 52% for Morison’s pouch.29
Characteristics for the RUQ may vary based on interpretation of physiologic or clinically significant free fluid. In the setting of clinically significant fluid, defined as moderate free fluid on abdominal computed tomography or if the patient went to the operating room, sensitivity of the RUQ has been reported to range from 52% to 70%, with specificity up to 96% to 100%.30-32
Pooled likelihood ratios (LRs) from pediatric studies suggest a positive LR of 17.3 and negative LR of 0.5, but these values vary significantly with operator experience and patient body habitus.33 In contrast to adults, where 200 mL to 400 mL of fluid may be required for reliable RUQ detection, the minimum detectable volume in children remains undefined, further complicating interpretation.34-38
Limitations include potential false positives from perinephric fat, fluid-filled bowel, or vessels, and false negatives in patients scanned too early after injury or with isolated pelvic bleeding. Serial FAST exams and clinical correlation remain essential, especially in equivocal cases. (See Figure 1.)
Figure 1. Normal FAST Right Upper Quadrant |
5-year-old female via curvilinear probe |
 |
FAST: Focused Assessment with Sonography for Trauma Image courtesy of: Matthew D. Holmes, MD. |
Left Upper Quadrant
The left upper quadrant (LUQ) view in the FAST exam is colloquially known as the “knuckles in the bed” view because of the often awkward probe position required to visualize the splenorenal recess, left pleural space, and inferior pole of the left kidney. This window can be technically challenging, especially in larger or uncooperative pediatric patients, because it typically requires the examiner to press deeply with the probe angled posteriorly beneath the rib cage. As such, the examiner’s hand or knuckles typically will push into the bed to achieve the appropriate window, hence its moniker. In children, the spleen is proportionally larger and more anteriorly positioned, which can facilitate acquisition of this view compared to adults.
The deepest space in the LUQ is the left subphrenic space, which underscores the importance of including the diaphragm in the field of view to detect intraperitoneal and pleural fluid. Anechoic fluid may collect between the spleen and diaphragm, spleen and kidney, or along the inferior pole of the spleen. Careful fanning through the coronal plane ensures adequate evaluation of these dependent spaces.
In pediatric patients, this view may demonstrate fluid tracking from the suprasplenic or splenorenal regions, although free fluid is less commonly isolated to the LUQ compared to the pelvis or RUQ.28 Still, when present, LUQ fluid is highly specific for significant injury and correlates most often with splenic injury, the most commonly injured solid organ in pediatric blunt abdominal trauma.39
Probe selection and technique are particularly important in this view. The curvilinear probe is standard, but a phased-array probe may be helpful in smaller patients or when rib spacing is limited. Gentle probe pressure is essential to avoid compression of underlying structures, and imaging in both longitudinal and transverse planes increases sensitivity.
While the LUQ view has a lower sensitivity in detecting isolated injuries when compared to the pelvic or RUQ windows, its inclusion remains critical, especially given the high incidence of splenic injuries in pediatric blunt trauma.31 In one study, the presence of LUQ free fluid was associated with a positive predictive value of 87% for intra-abdominal injury requiring intervention.29 (See Figure 2.)
Figure 2. Normal FAST Left Upper Quadrant |
5-year-old female via curvilinear probe |
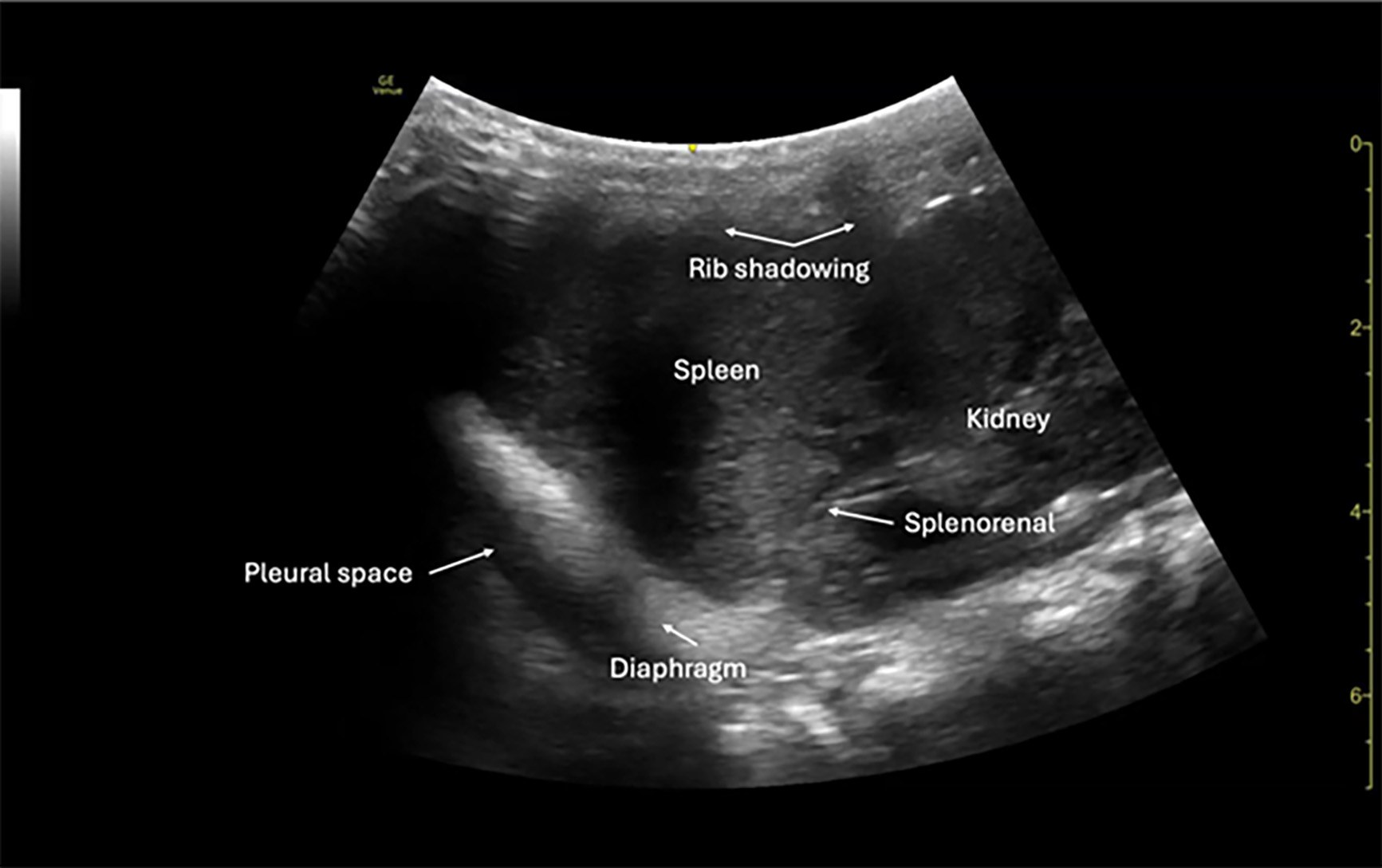 |
FAST: Focused Assessment with Sonography for Trauma Image courtesy of: Matthew D. Holmes, MD. |
Subxiphoid
The subxiphoid (also called subcostal) view in pediatric trauma can be obtained in one of two ways. One is by placing the phased array or curvilinear probe directly over the epigastric area and angling superiorly toward the left shoulder beneath the rib cage, and the other is by placing the probe directly on the anterior chest wall, especially when abdominal tenderness or guarding precludes the subcostal approach. The choice of technique is influenced by patient body habitus, injury pattern, and comfort. In smaller children or infants, subxiphoid imaging often is more successful because of relatively compliant abdominal walls and less rib ossification.31
This view is used primarily to assess for pericardial effusion, which may indicate cardiac injury or tamponade physiology in the setting of blunt or penetrating trauma. The goal is to obtain a complete four-chamber view of the heart to evaluate for anechoic fluid surrounding the myocardium, typically appearing between the posterior pericardium and right ventricle.38 It also is helpful for assessing right ventricular collapse, chamber compression, or a “swinging heart” in cases of tamponade.
A pericardial effusion causing tamponade physiology is rare but life-threatening and its detection is a critical component of the FAST exam. Focused cardiac ultrasound has a sensitivity of about 96% and specificity of 98% to 100% for detecting pericardial effusion, although these values may vary depending on the clinician.40 Early identification of pericardial blood can prompt rapid intervention, such as pericardiocentesis or surgical exploration.41
Probe orientation is variable since the main focus is identification of a pericardial effusion. ATLS teaches that the probe marker is directed to the patient’s right, while the majority of cardiac windows are obtained with the marker directed toward the patient’s left. Regardless, a generous amount of gel should be used to improve image acquisition through abdominal structures such as the liver. In uncooperative or unstable patients, image acquisition may be limited; however, even partial visualization of the pericardial space can be diagnostically useful. (See Figure 3.)
Figure 3. Normal FAST Subxiphoid View |
5-year-old female via phased array probe |
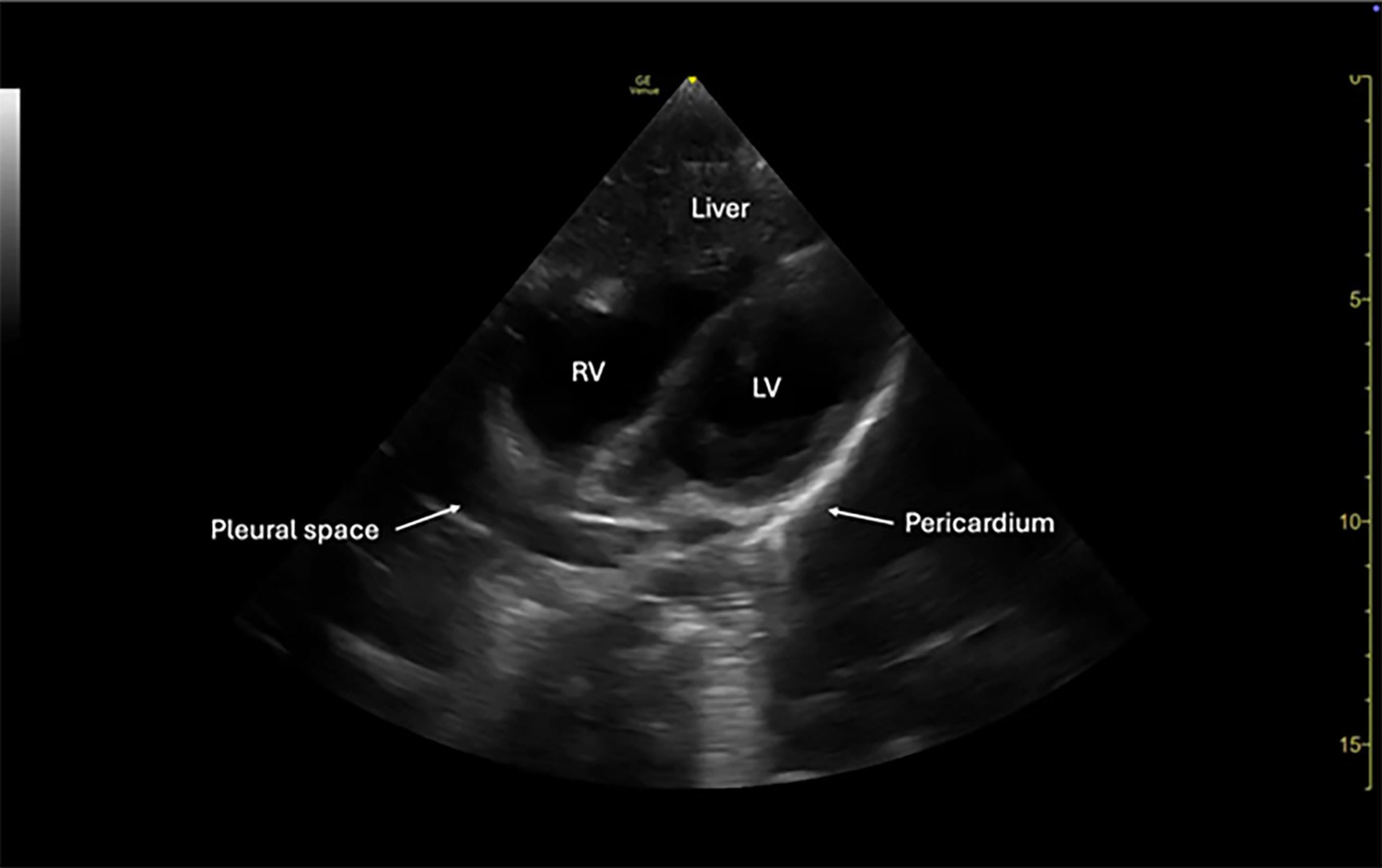 |
FAST: Focused Assessment with Sonography for Trauma Image courtesy of: Matthew D. Holmes, MD. |
Suprapubic
The suprapubic view is obtained by placing either a phased array or curvilinear probe just superior to the pubic symphysis and angling inferiorly into the pelvis, with the probe marker oriented to the patient’s right for the transverse view. A second view should be acquired by rotating the probe 90 degrees (at this point the marker would be toward the patient’s head) for a longitudinal view. This dual-plane approach increases sensitivity and ensures proper evaluation of the rectovesical (in males) or rectouterine/pouch of Douglas (in females) spaces, where intraperitoneal fluid may first accumulate.
Among all FAST windows, the pelvic view is the most sensitive for detecting free intraperitoneal fluid in pediatric trauma, likely due to the relatively deep, midline location and the tendency of fluid to collect in gravity-dependent spaces.30 In contrast to adults, where Morison’s pouch is the earliest site of fluid accumulation, pediatric studies have shown that the pelvis is the first location to demonstrate free fluid in up to 66% to 85% of positive exams.28
Sonographic findings include anechoic fluid collecting in the posterior pelvis, outlining bladder margins, or pooling between the bladder and uterus in females. Small volumes can be missed if the bladder is decompressed, so it is ideal to scan when the bladder is partially distended.31 There is no established minimum fluid volume threshold for detection in pediatric patients, since values vary with body size, bladder filling, and probe resolution.
Limitations of this view include inadequate bladder filling, bowel gas artifact, and patient discomfort, which can affect image quality. Using a gentle technique and maintaining good probe contact with ample gel can improve visualization. As stated, a full bladder also may enhance diagnostic accuracy by serving as an acoustic window to the posterior pelvic space.29
Overall, the suprapubic view plays a critical role in pediatric trauma ultrasonography, especially when other FAST windows are equivocal or limited by anatomy or body habitus. Its inclusion is vital in detecting clinically significant hemoperitoneum, particularly in children with isolated lower abdominal injury or delayed presentation. (See Figure 4.)
Figure 4. Normal FAST Suprapubic View |
3-year-old male via curvilinear probe |
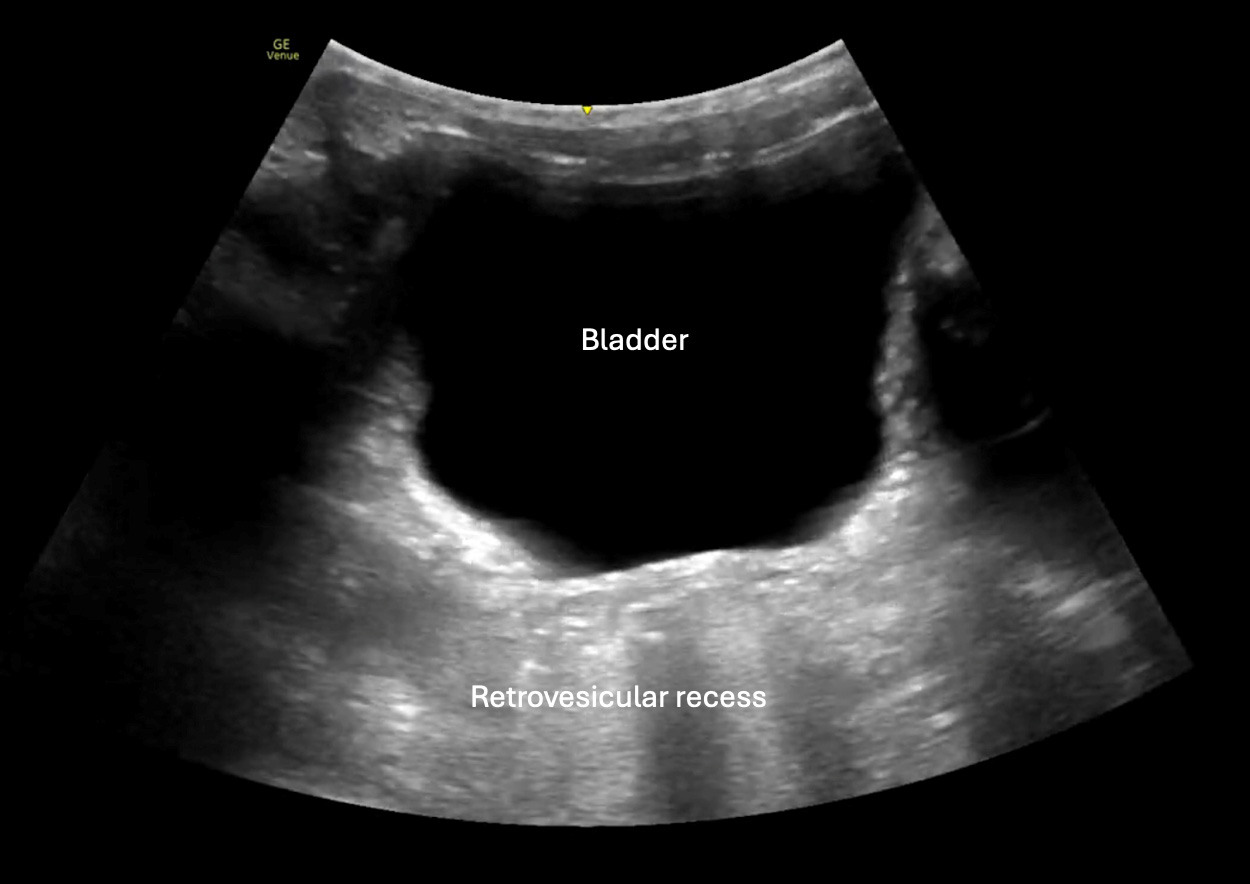 |
FAST: Focused Assessment with Sonography for Trauma Image courtesy of: Matthew D. Holmes, MD. |
Lung View
The lung view in the E-FAST is obtained by placing a high-frequency linear probe or a phased array probe in the midclavicular line at the second or third intercostal space on the anterior chest wall, typically with the probe marker oriented toward the patient’s head. This view is used to rapidly evaluate for pneumothorax, hemothorax, or other causes of lung collapse. In pediatric patients, where chest wall compliance is higher and auscultation may be less reliable in noisy environments, lung ultrasound offers a highly sensitive and radiation-free method of assessment.40
The hallmark of a normal lung exam is the presence of lung sliding, which is the horizontal motion generated by the visceral and parietal pleura sliding against one another. This can be visualized in real-time (B-mode) or confirmed with M-mode, where normal lung movement produces the classic “seashore sign” (a granular pattern beneath a smooth superficial line). In the case of pneumothorax, lung sliding will be absent, and M-mode will instead reveal the “barcode sign” or “stratosphere sign,” indicating no pleural movement.42 In pediatric trauma patients, particularly when radiation exposure is a concern, lung ultrasound has demonstrated a sensitivity of up to 86% to 100% and specificity of 94% to 100% for pneumothorax when performed by trained operators.43 It also outperforms chest X-ray for the early detection of pneumothorax and pleural fluid in trauma settings.44
While lung sliding rules out pneumothorax in the scanned region, its absence is not specific and also may be seen in mainstem intubation, pleural adhesions, or apnea. To improve diagnostic accuracy, additional findings, such as the presence or absence of B-lines (comet tail artifacts) and the lung point (transition between sliding and non-sliding pleura), should be assessed since detection of the lung point is highly specific for pneumothorax.45
The use of lung views as part of the E-FAST exam is particularly valuable in children, where rapid, noninvasive assessment for thoracic injury is critical and where traditional imaging modalities may be delayed or technically limited. Ultrasound should be performed in bilateral anterior and lateral chest zones to improve diagnostic yield, and its integration into trauma protocols can expedite decision-making in unstable pediatric patients. (See Figure 5.)
Figure 5. Normal FAST Lung View |
3-year-old male via M-mode using a linear probe |
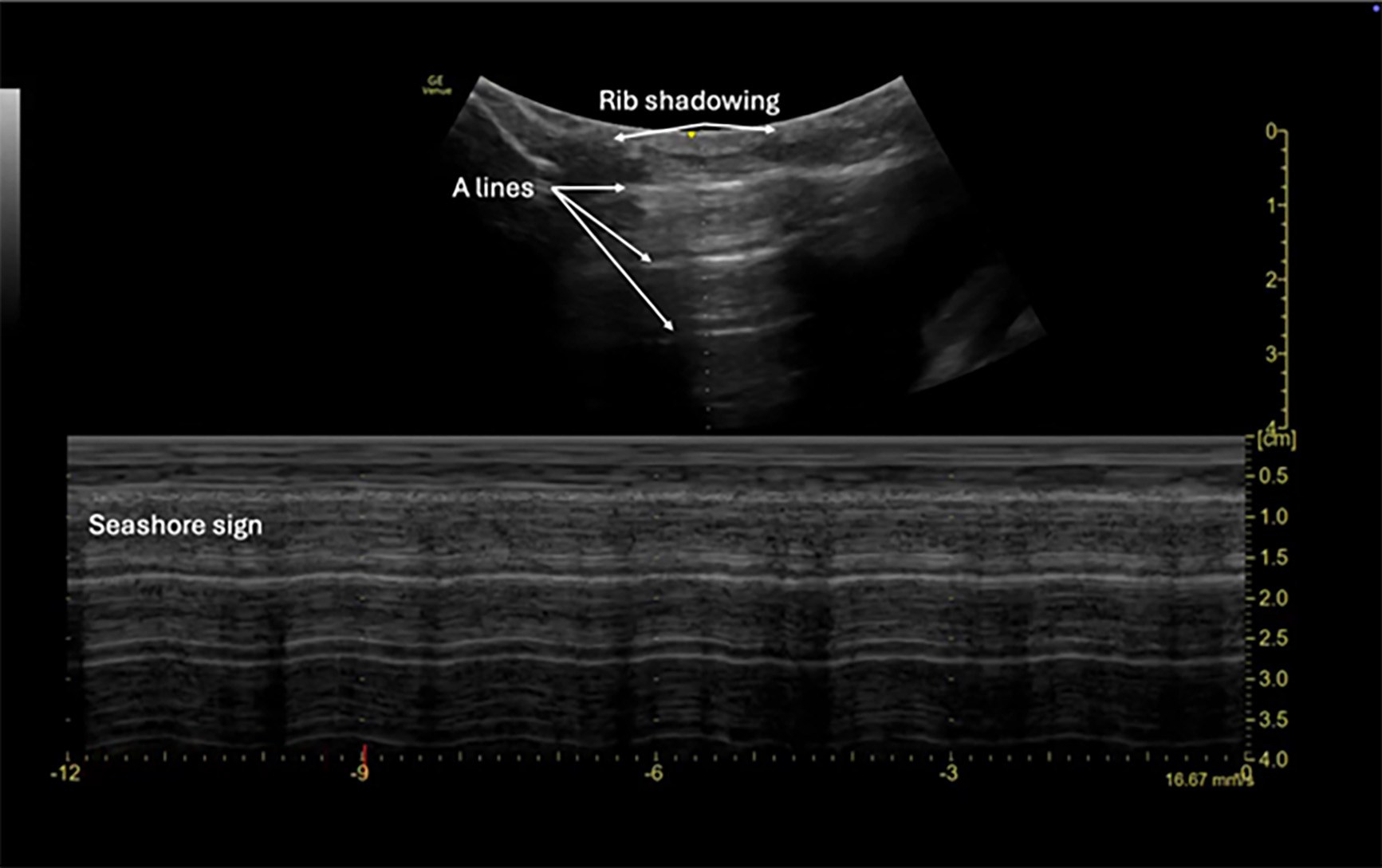 |
FAST: Focused Assessment with Sonography for Trauma Image courtesy of: Matthew D. Holmes, MD. |
Additional Areas of Utility
Musculoskeletal Assessment
Most commonly, musculoskeletal injuries are diagnosed using a combination of physical exam and plain film imaging. Ultrasound provides a dynamic tool to assess both pediatric joints and long bones for signs of injury. When using ultrasound in the detection of long bone fractures, it was found to have a sensitivity and specificity of 95.3% and 85.5%, respectively.46-48 Ultrasound also was able to identify the need for fracture reduction with a sensitivity of 100%.48 Ultrasound has been used for joint assessment, especially with the hip joint, to diagnose joint effusion, developmental hip dysplasia, transient synovitis, or juvenile idiopathic arthritis, among others.49 Traumatic injury to the shoulder or hip also can be assessed using ultrasound.
The probe of choice when evaluating musculoskeletal injuries usually is the linear probe, although the curvilinear probe may be necessary depending on body habitus. Different layers of tissue can be identified on ultrasound to determine where pathology is present. Bone can be identified usually deep to these structures depending on the location and will appear hyperechoic (brighter) than the surrounding structures.
Shoulder
Ultrasound is an increasingly valuable imaging modality in the evaluation of pediatric shoulder injuries, particularly in trauma settings where rapid, radiation-free assessment is preferred. Children present unique challenges in musculoskeletal imaging because of open growth plates (physis), increased cartilage content, and variable ossification, which may limit the sensitivity of traditional radiography for detecting subtle injuries. The shoulder area is a common site of injury in active children, with clavicle fractures, proximal humeral fractures, and anterior shoulder dislocations, respectively, being most common.50
Ultrasound can effectively identify glenohumeral dislocations and subtle fractures in the pediatric population. Identification of shoulder dislocations was associated with a sensitivity of 99.1% and specificity of 99.2% when performed by trained providers or technicians.51 Regarding fractures, ultrasound is particularly useful for detecting cortical disruption of the humeral head or clavicle, although its sensitivity for subtle or intra-articular fractures may be lower compared to radiography depending on the interpreting provider.52
In children, the presence of cartilaginous structures and growth plates, such as the proximal humeral physis, can be mistaken for fracture lines or dislocation unless properly recognized. Familiarity with normal ossification centers is crucial to avoid misinterpretation.53
The posterior approach to shoulder ultrasound is the preferred technique for evaluating suspected dislocations. With the patient seated or in the lateral decubitus position, place a high-frequency linear probe transversely on the posterior aspect of the shoulder, just inferior to the scapular spine. The probe marker should point laterally. Identify the glenoid fossa and humeral head. In a normal (reduced) shoulder, the humeral head will sit congruently within the glenoid. (See Figures 6 and 7.) In an anterior dislocation, the humeral head will appear displaced anteriorly (and thus deeper on the screen), while in a posterior dislocation it will lie posteriorly and more superficial.
Figure 6. Normal Shoulder View |
3-year-old male via linear probe |
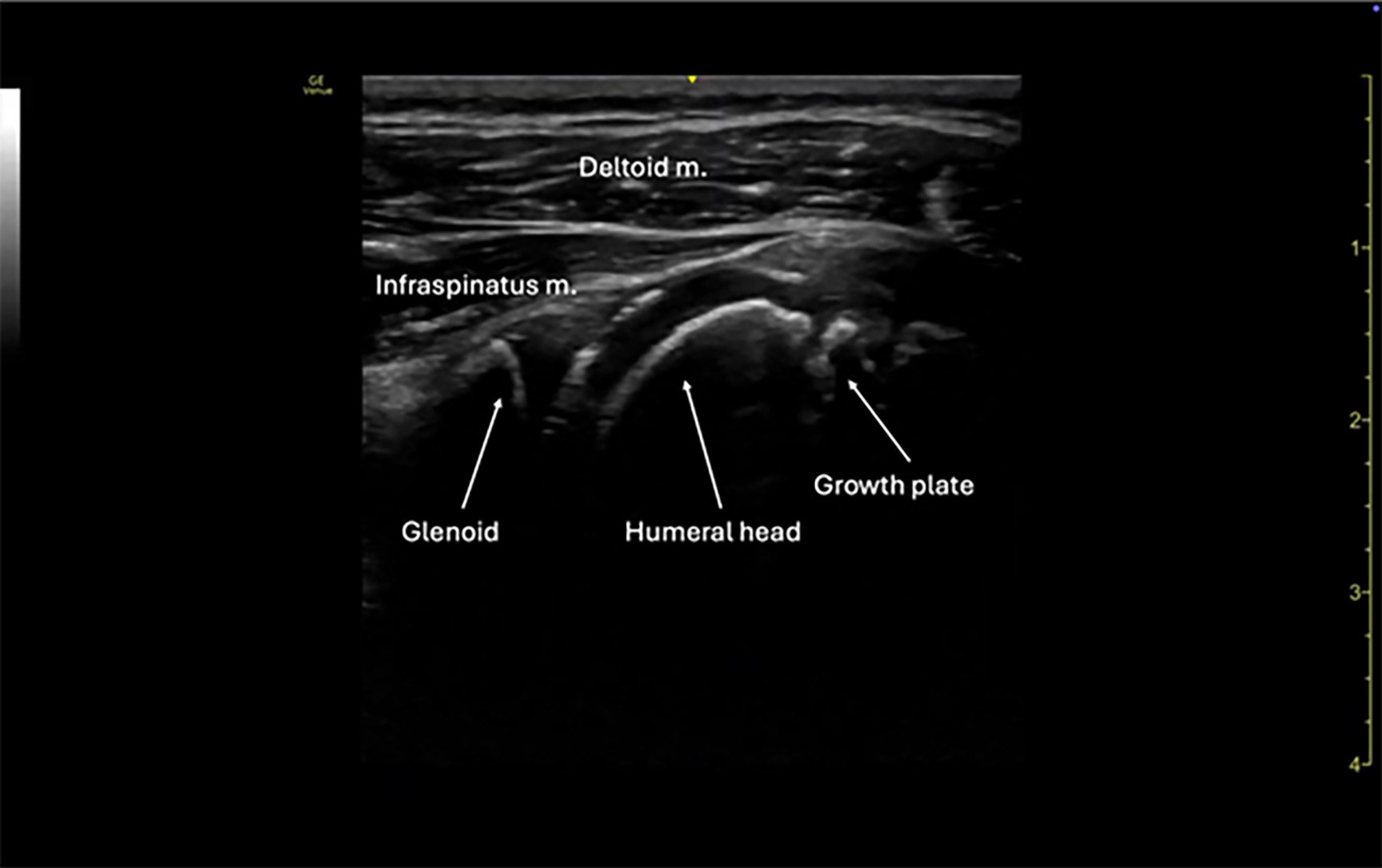 |
Image courtesy of: Matthew D. Holmes, MD. |
Figure 7. Normal Shoulder View |
5-year-old female via linear probe |
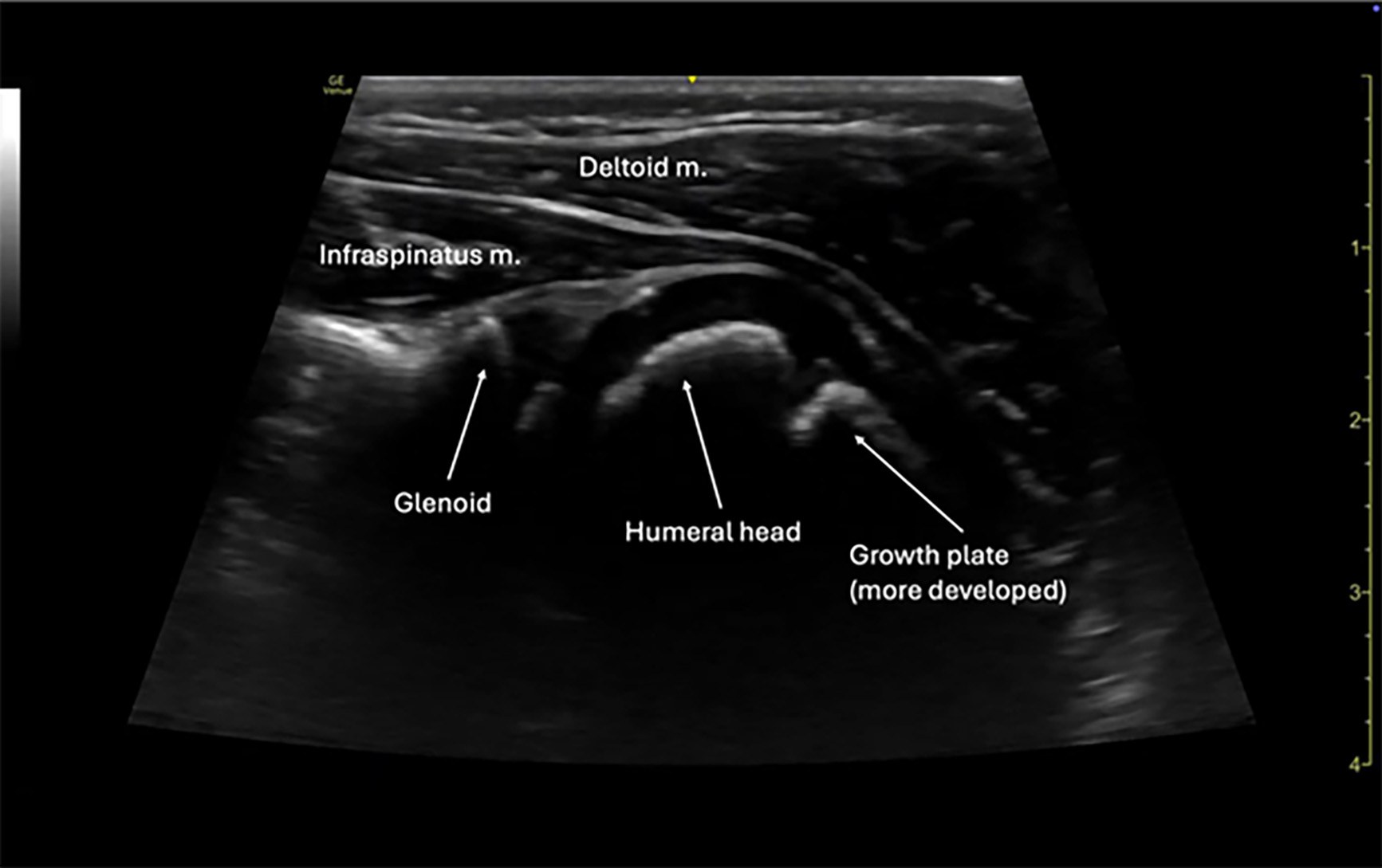 |
Image courtesy of: Matthew D. Holmes, MD. |
Long Bone
The use of ultrasound for diagnosing long bone fractures is fairly accurate when compared to routine plain film images. Ultrasound was found to have an accuracy of 91.2% for detecting long bone fractures, with a sensitivity of 100%.49 The high-frequency linear transducer is the preferred probe to use when evaluating for long bone fractures. The curvilinear probe may be used for deeper bones but is slightly limited in clarity.
On ultrasound, bone should appear as a hyperechoic structure without disruption. Fractures will be represented as a disruption in this hyperechoic structure. Surrounding areas of trauma also can be identified using ultrasound to help the user better identify a bony image such as soft tissue swelling or presence of a hematoma. This tool can be extremely useful in fractures that are common in children, such as greenstick fractures that may be difficult to identify on plain film imaging and may be subtle. The accuracy of ultrasound when identifying fractures can be improved by using techniques such as a water bath or copious gel to improve image quality and accuracy. This also will allow the user to place less pressure on the injured area and usually allows the patient to be more compliant with the evaluation.
Foreign Body
Ultrasound can be useful in identifying retained foreign bodies within the soft tissue. Plain films help identify radiopaque foreign bodies, but ultrasound can be helpful with both radiopaque and radio-translucent foreign bodies.46 The high-frequency linear transducer is the preferred probe to be used when evaluating for a foreign body. It also is important to evaluate the structure in more than one plane, similar to the importance of obtaining more than one X-ray view if possible. All foreign bodies will appear hyperechogenic when compared to the surrounding soft tissue, and some may show artifact as well in the form of posterior acoustic shadowing, reverberation, or a hypoechoic rim.46 The denser the foreign body is, the more hyperechogenic it will appear on ultrasound.
It is important to be aware of some false positives that may occur when using ultrasound to evaluate a foreign body. These include calcifications, scar tissue, hematomas, and air. Therefore, it is important to use ultrasound in conjunction with physical examination, clinical story, and other imaging modalities such as X-ray.49
Vascular Access
Obtaining vascular access is extremely important, especially in the trauma patient. Pediatric patients already provide an added challenge with the size of their anatomy, but this can be compounded in the setting of shock. Ultrasound increases first-attempt success rates and decreases the time it takes to obtain vascular access on pediatric patients.54 The linear probe is best used for vascular access because it provides the best clarity of superficial structures.55,56 This can be used for peripheral venous access, central venous access, or arterial access. Use the ultrasound to scan the area you are looking for a vessel. In the case of peripheral access, starting in the antecubital fossa and moving distally toward the forearm is a good approach. Once a vessel is identified, visual assessment, color flow, or Doppler can be used to determine if the vessel is arterial or venous. Usually, veins will be easily compressible, while arteries will pulsate and not completely compress. However, in pediatric patients, especially hypotensive pediatric patients, this is not always a reliable test. Doppler mode will provide visual and auditory confirmation of the vessel’s status. Color mode shows blood moving toward or away from the probe using blue and red differentiation but also will show pulsatile blood flow with a visual “flashing” of that color on the ultrasound screen.
Once the vessel is identified, ultrasound is used in real time to directly visualize the needle, and ultimately the catheter, entering the vessel. After the skin is prepped, the vessel should be lined up in the middle of the ultrasound screen, allowing the user to ensure the needle is entering the skin just over the vessel. Once the needle penetrates the first layer of skin, the user will identify the needle tip as a hyperechoic structure within the tissue. After identifying this, the user will slowly advance the needle, while keeping the ultrasound on the needle tip until it is visualized entering the desired blood vessel. After the vessel has been entered, the user usually will continue to track the needle tip a few more millimeters into the vessel to avoid going through the vessel or having the needle come out of the vessel on catheter insertion. Once the catheter is in place, this also can be visualized on ultrasound.
Nerve Block
Pain control is an important aspect in patient care, particularly in trauma patients. Nerve blocks provide another modality of pain control and can be used in pediatric patients with the help of ultrasound. Benefits of this modality include the lack of ionizing radiation and overall lower amounts of local anesthetic used, which lowers the risk of toxicity and allows for multiple blocks, if necessary.57,58 Nerve blocks are gaining more attention for surgical analgesia and are increasingly used by emergency medicine providers for injuries with difficult pain profiles, such as femur fractures, extensive lacerations, or rib fractures. Because of the limitations of this article, all the various types and options for nerve blocks will not be discussed. The technique of the fascia iliaca block will be discussed.
Fascia Iliaca Block
This block is used for injuries to the thigh and knee and has been shown to have improved pain relief over opioid analogs in pediatric patients with femur fractures.58 This block covers the anatomical area of the femur, proximal tibia, patella, and the tissue of the anterior thigh. This block should not be performed if there is infection over the injection site, an anesthetic allergy, potential for compartment syndrome, the patient is younger than 2 years of age, or there are signs of neurovascular injury.58
Supplies needed for this block include:
- Sterile ultrasound gel;
- Chlorhexidine or equivalent;
- 22-gauge spinal needle with attached tubing primed with sterile saline;
- Local anesthetic based on the patient’s ideal body weight;
- 10-20 mL syringe depending on patient weight;
- Sterile saline flushes.
When choosing an anesthetic for a nerve block, time to pain relief and length of pain relief should be considered. Lidocaine provides the fastest onset but the shortest duration, while ropivacaine and bupivacaine provide longer pain relief but a slower onset. Ropivacaine is the preferred anesthetic for this block because it is less lipophilic, has less risk of neurologic or cardiac toxicity, and provides long-lasting pain relief.58 Dosages will vary based on the patient’s weight and, thus, should be confirmed with appropriate calculations based on each specific agent used.
The fascia iliaca block begins by identifying the fascia iliaca on ultrasound. The target region lies within the groin, deep to the femoral artery, vein, and nerve. Before initiating the procedure, it is essential to perform and document a thorough neurovascular examination of all areas to be anesthetized, since sensory and motor assessments will be limited following successful analgesia. Position the patient supine, with the hip and knee in a neutral, neither flexed nor extended, position. External rotation of the hip may facilitate improved sonographic visualization. Depending on the child’s age and level of cooperation, consider using child life specialists, involving family members, or administering pharmacologic anxiolysis (e.g., midazolam) to optimize patient comfort and procedural success. A high-frequency linear transducer should be selected, preferably one with a broad footprint to maximize anatomical visualization during the block. Once the patient is appropriately positioned, place the transducer parallel to the inguinal canal on the side requiring analgesia. Orient the probe marker toward the patient’s right side. The needle should be introduced in-plane from the lateral aspect
Once the probe is placed, identification of anatomy should be confirmed using the following landmarks: sartorius muscle, iliopsoas muscle, fascia lata, fascia iliaca, and the femoral artery, vein, and nerve.
After landmarks are identified, the subcutaneous tissue can be anesthetized before needle insertion. After piercing the skin, identify the needle tip with the ultrasound prior to additional movements to ensure the needle does not enter into the wrong structure. The needle tip will then be tracked through the tissue to pierce the fascia iliaca. Normal saline can be used to hydrodissect and ensure the needle tip is in the desired location prior to anesthetic administration. Apply negative pressure by pulling back on the syringe to ensure the needle is not within a vessel. Once the needle is in the correct location, the remaining anesthetic can be administered in small aliquots. The patient should be kept on the cardiac monitor for at least 30 minutes but up to four hours following the nerve block to evaluate for cardiotoxicity/arrhythmias. The patient should be re-evaluated to determine the efficacy of the block.
Conclusion
Point-of-care ultrasound is a critical, radiation-free tool in the evaluation and management of pediatric trauma, enabling rapid bedside assessment of life-threatening injuries. Its applications extend beyond the FAST exam to include vascular access, fracture identification, and regional anesthesia, such as the fascia iliaca block. While operator skill and patient factors may limit sensitivity in some cases, ultrasound remains an essential adjunct in optimizing pediatric trauma care.
Matthew D. Holmes, MD, is Emergency Medicine Resident, Chief, Dayton Children’s Emergency Department, Wright State University Boonshoft School of Medicine, Dayton, OH.
Lucy Hale, DO, is Emergency Medicine Resident, Wright State University Boonshoft School of Medicine, Dayton, OH.
Titus Chu, MD, is Assistant Professor, Emergency Medicine, Wright State University Boonshoft School of Medicine, Dayton, OH.
References
1. Centers for Disease Control and Prevention. WISQARS Leading Causes of Death Reports. https://wisqars.cdc.gov
2. Yoshida T, Yoshida T, Noma H, et al. Diagnostic accuracy of point-of-care ultrasound for shock: A systematic review and meta-analysis. Crit Care. 2023;27:200.
3. Campbell S. A short history of sonography in obstetrics and gynaecology. Facts Views Vis Obgyn. 2013;5(3):213-229.
4. American College of Surgeons. Advanced Trauma Life Support for Physicians. American College of Surgeons; 1997.
5. Diercks DB, Mehrotra A, Nazarian DJ, et al. Clinical policy: Critical issues in the evaluation of adult patients presenting to the emergency department with acute blunt abdominal trauma. Ann Emerg Med. 2011;57(4):387-404.
6. Lentz KA, McKenney MG, Nuñez DB, Martin L. Evaluating blunt abdominal trauma: Role for ultrasonography. J Ultrasound Med. 1996;15(6):447-451.
7. Hoff WS, Holevar M, Nagy KK, et al. Practice management guidelines for the evaluation of blunt abdominal trauma: The EAST Practice Management Guidelines Work Group. J Trauma. 2002;53(3):602-615.
8. Akgür FM, Aktuğ T, Kovanhkaya A, et al. Initial evaluation of children sustaining blunt abdominal trauma: Ultrasonography vs. diagnostic peritoneal lavage. Eur J Pediatr Surg. 1993;3(5):278-280.
9. Katz S, Lazar L, Rathaus V, Erez I. Can ultrasonography replace computed tomography in the initial assessment of children with blunt abdominal trauma? J Pediatr Surg. 1996;31(5):649-651.
10. Stengel D, Leisterer J, Ferrada P, et al. Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Database Syst Rev. 2018;12:CD012669.
11. Smith-Bindman R. Environmental causes of breast cancer and radiation from medical imaging: Findings from the Institute of Medicine report. Arch Intern Med. 2012;172(13):1023-1027.
12. Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukemia and brain tumors: A retrospective cohort study. Lancet. 2012;380(9840):499-505.
13. Brenner DJ, Hall EJ. Computed tomography — an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277-2284.
14. Netherton S, Milenkovic V, Taylor M, Davis PJ. Diagnostic accuracy of eFAST in the trauma patient: A systematic review and meta-analysis. CJEM. 2019;21(6):727-738.
15. McGahan JP, Schick MA, Mills L. Fundamentals of Emergency Ultrasound. 1st ed. Elsevier; 2019.
16. Middlemore Emergency Medicine Education. Probecraft. https://www.mmheme.org/knobology
17. Heart Medical. 7 most common ultrasound probe & transducers types. Aug. 2, 2024. https://www.heartmedical.com/blogs/news/7-most-common-ultrasound-probe-transducers-types
18. American College of Surgeons Committee on Trauma. ATLS®: Advanced Trauma Life Support Student Course Manual. 10th ed. American College of Surgeons; 2018.
19. Calder BW, Vogel AM, Zhang J, et al. Focused assessment with sonography for trauma in children after blunt abdominal trauma: A multi-institutional analysis. J Trauma Acute Care Surg. 2017;83(2):218-224.
20. Fox JC, Boysen M, Gharahbaghian L, et al. Test characteristics of focused assessment of sonography for trauma for clinically significant abdominal free fluid in pediatric blunt abdominal trauma. Acad Emerg Med. 2011;18(5):477-482.
21. Liang T, Roseman E, Gao M, Sinert R. The utility of the focused assessment with sonography in trauma examination in pediatric blunt abdominal trauma: A systematic review and meta-analysis. Pediatr Emerg Care. 2021;37(2):108-118.
22. Policy Statement — Principles of pediatric patient safety: Reducing harm due to medical care. Pediatrics. 2011;127(6):1199-1210.
23. Rozycki GS, Ballard RB, Feliciano DV, et al. Surgeon-performed ultrasound for the assessment of truncal injuries: Lessons learned from 1540 patients. Ann Surg. 1998;228(4):557-567.
24. Branney SW, Wolfe RE, Moore EE, et al. Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid. J Trauma. 1995;39:375-380.
25. Arredondo AR, Wilkinson M, Barber RB, et al. Ultrasonographic evaluation of physiologic free intraperitoneal fluid in healthy children: A prospective observational study. J Ultrasound Med. 2022;41(5):1061-1067.
26. Fornari MJ, Lawson SL. Pediatric blunt abdominal trauma and point-of-care ultrasound. Pediatr Emerg Care. 2021;37(12):624-629.
27. Kaur G, Kaur T, Das CJ. Morrison’s pouch: Anatomy and radiological appearance of pathological processes. Indian J Radiol Imaging. 2022;33(1):80-88.
28. Scaife ER, Rollins MD, Barnhart DC, et al. The role of focused abdominal sonography for trauma (FAST) in pediatric trauma evaluation. J Pediatr Surg. 2013;48(6):1377-1383.
29. Holmes JF, Kelley KM, Wootton-Gorges SL, et al. Effect of abdominal ultrasound on clinical care, outcomes, and resource use among children with blunt torso trauma: A randomized clinical trial. JAMA. 2017;317(22):2290-2296.
30. Sola JE, Cheung MC, Yang R, et al. Pediatric FAST and elevated liver transaminases: An effective screening tool in blunt abdominal trauma. J Surg Res. 2009;157(1):103-107.
31. Menaker J, Blumberg S, Wisner DH, et al; Intra-abdominal Injury Study Group of the Pediatric Emergency Care Applied Research Network (PECARN). Use of the focused assessment with sonography for trauma (FAST) examination and its impact on abdominal computed tomography use in hemodynamically stable children with blunt torso trauma. J Trauma Acute Care Surg. 2014;77(3):427-432.
32. Fischer JW, Sivitz AB, Abo AM. Pediatric applications. Radiology Key. Dec. 27, 2016. https://radiologykey.com/pediatric-applications/
33. Riera A, Hayward H, Torres Silva C, Chen L. Reevaluation of FAST sensitivity in pediatric blunt abdominal trauma patients: Should we redefine the qualitative threshold for significant hemoperitoneum? Pediatr Emerg Care. 2021;37(12):e1012-e1019.
34. Ma OJ, Mateer JR, Ogata M, et al. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38(6):879-885.
35. Rowland-Fisher A, Reardon RF. E-FAST (extended focused assessment with sonography in trauma). In: Sonoguide. American College of Emergency Physicians. Oct. 19, 2021. https://www.acep.org/sonoguide/basic/fast
36. American College of Emergency Physicians. Focused Assessment with Sonography for Trauma (FAST). Sonoguide website. Oct. 19, 2021. https://www.acep.org/sonoguide/basic/fast
37. Savatmongkorngul S, Wongwaisayawan S, Kaewlai R. Focused assessment with sonography for trauma: Current perspectives. Open Access Emerg Med. 2017;9:57-62.
38. Rozycki GS, Ochsner MG, Jaffin JH, Champion HR. Prospective evaluation of surgeons’ use of ultrasound in the evaluation of trauma patients. J Trauma. 1993;34(4):516-527.
39. Gaines BA. Intra-abdominal solid organ injury in children: Diagnosis and treatment. J Trauma. 2009;67(2 Suppl):S135-S139.
40. Bloom BA, Gibbons RC. Focused Assessment with Sonography for Trauma (FAST). In: StatPearls. StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK470479
41. Kovacevic M, Cooper JM, Krater R. Point-of-care ultrasound in early identification of tamponade: A case series. Cureus. 2025;17(2):e78823.
42. Volpicelli G, Elbarbary M, Blaivas M, et al; International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38(4):577-591.
43. Vasquez DG, Berg GM, Srour SG, Ali K. Lung ultrasound for detecting pneumothorax in injured children: Preliminary experience at a community-based Level II pediatric trauma center. Pediatr Radiol. 2020;50(3):329-337.
44. Desai N, Harris T. Extended focused assessment with sonography in trauma. BJA Educ. 2018;18(2):57-62.
45. Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest. 2008;134(1):117-125.
46. Marín-Díez E, Landeras Álvaro RM, Lamagrande Obregón A, et al. Ultrasonography of subcutaneous foreign bodies: Differences depending on their nature, complications, and potential diagnostic errors. Radiología (English Edition). 2020;62(1):3-12.
47. Rabiner JE, Friedman LM, Khine H, et al. Accuracy of point-of-care ultrasound for diagnosis of fractures in children and young adults. Pediatr Emerg Care. 2013;29(5):546-549.
48. Kang YR, Koo J. Ultrasonography of the pediatric hip and spine. Ultrasonography. 2017;36(3):239-251.
49. Bahl A, Bagan M, Joseph S, Brackney A. Comparison of ultrasound and plain radiography for the detection of long-bone fractures. J Emerg Trauma Shock. 2018;11(2):115-118.
50. Chen FS, Diaz VA, Loebenberg M, Rosen JA. Shoulder and elbow injuries in the skeletally immature athlete. J Am Acad Orthop Surg. 2005;13:172-185.
51. Attard Biancardi MA, Jarman RD, Cardona T. Diagnostic accuracy of point-of-care ultrasound (PoCUS) for shoulder dislocations and reductions in the emergency department: A diagnostic randomised control trial (RCT). Emerg Med J. 2022;39(9):655-661.
52. Weinberg ER, Tunik MG, Tsung JW. Accuracy of clinician-performed point-of-care ultrasound for the diagnosis of fractures in children and young adults. Injury. 2010;41(8):862-868.
53. Zember J, Vega P, Rossi I, Rosenberg ZS. Normal development imaging pitfalls and injuries in the pediatric shoulder. Pediatr Radiol. 2019;49(12):1617-1628.
54. Doniger SJ, Ishimine P, Fox JC, Kanegaye JT. Randomized controlled trial of ultrasound-guided peripheral intravenous catheter placement versus traditional techniques in difficult-access pediatric patients. Pediatr Emerg Care. 2009;25:154-159.
55. Schmidt GA, Blaivas M, Conrad SA, et al. Ultrasound-guided vascular access in critical illness. Intensive Care Med. 2019;45(4):434-446.
56. Roberts S. Peripheral Nerve Blocks for Children. NYSORA. https://www.nysora.com/topics/sub-specialties/pediatric-anesthesia/peripheral-nerve-blocks-children/
57. Wathen JE, Gao D, Merritt G, et al. A randomized controlled trial comparing a fascia iliaca compartment nerve block to a traditional systemic analgesic for femur fractures in a pediatric emergency department. Ann Emerg Med. 2007;50(2):162-171, 171.e1.
58. Kangwa M, Shaahinfar A. PEM POCUS Series: Pediatric Ultrasound Fascia Iliaca Block. Academic Life in Emergency Medicine. April 6, 2022. https://www.aliem.com/pem-pocus-series-pediatric-ultrasound-fascia-iliaca-block/