
The Seasonal Surge: Influenza in the ED
October 15, 2025
By Michael Ullo, MD, MHCI, FACEP, and Gregory Sugalski, MD, MBA
Executive Summary
- The most recent influenza season was the worst since 2017-2018, and current projections suggest the upcoming season will be similarly severe. Emergency providers should anticipate high emergency department (ED) volume and hospitalizations.
- Classic influenza typically presents with abrupt-onset fever, myalgias, and headache followed by cough or sore throat; however, older adult patients may present atypically with generalized weakness or altered mental status, while children may have gastrointestinal symptoms.
- Influenza A dominated the recent season, accounting for 88.8% of positive specimens, while overall hospitalizations were most significant in patients aged 65 years and older.
- Molecular assays (polymerase chain reaction/nucleic acid amplification tests) represent the gold standard for influenza diagnosis and are rapidly available in the emergency setting.
- Supportive care, including antipyretics, hydration, and oxygen as needed, remains the cornerstone of ED management.
- Antiviral treatment provides the greatest benefit when initiated for high-risk patients within the first 48 hours of symptom onset. When it is clinically indicated, oseltamivir remains the first-line agent.
- Low-risk, clinically stable patients may be discharged safely with education and strict return precautions; however, those with hypoxia, altered mental status, persistent vomiting, or at high risk for clinical decompensation should be considered for observation or admission.
- Emergency clinicians should remain vigilant for influenza-related complications, including secondary bacterial pneumonia, myocardial ischemia, and myocarditis.
- Vaccination remains the most effective preventive strategy against severe influenza, and emergency providers should continue to recommend vaccination to unvaccinated patients, especially those at a higher risk for severe disease.
Introduction
As winter approaches, it is time for healthcare providers to refocus on the recognition and management of the influenza virus. According to the Centers for Disease Control and Prevention (CDC), the 2024-2025 influenza season was classified as the most severe season since 2017-2018. Emergency departments continued to see a high number of visits for influenza-related illness, and cumulative hospitalization rates were the highest since the 2010-2011 influenza season. Patients at extremes of age experienced significant morbidity and mortality during the influenza season. Pediatric patients were especially vulnerable, with the highest number of influenza-associated pediatric deaths on record since tracking began in 2004. Older adult patients (age 65 years and older) had a higher hospitalization rate, further highlighting the significant impact the virus can have on the hospital setting.1,2
As the 2025-2026 influenza season commences in the Northern Hemisphere, healthcare providers must plan for a significant viral presence. Current weekly surveillance data show seasonal influenza activity is low nationally, consistent with the early fall period. However, the CDC’s outlook for the combined respiratory season (influenza, COVID-19, and respiratory syncytial virus [RSV]) predicts the peak combined hospitalization rate likely will be similar to that of last year, underscoring the potential for substantial demand on health systems. All flu vaccines for the 2025-2026 season are formulated as trivalent to target the expected circulating strains, further reinforcing the critical message for universal vaccination as the most effective mitigation strategy.3,4
Background
Influenza is an acute respiratory illness responsible for significant seasonal epidemics each year. The disease is transmitted by the influenza virus, an enveloped ribonucleic acid (RNA) virus in the Orthomyxoviridae family. Despite commonly being a self-limited illness, the virus causes significant morbidity and mortality each year.
Influenza A and influenza B are responsible for most clinically significant influenza infections. Influenza A is primarily implicated in notable pandemics that significantly affect public health. This virus is typed according to the antigenic characteristics of envelope glycoproteins, specifically hemagglutinin and neuraminidase. Influenza A has three major subtypes of hemagglutinin (H1, H2, and H3), along with two subtypes of neuraminidase (N1 and N2). (See Figure 1.)
Figure 1. Influenza Virus |
 |
Source: CDC/Douglas Jordan; Dr. Ruben Donis, Dr. James Stevens, Dr. Jerry Tokars, Influenza Division |
Influenza A and B cause nearly identical symptoms, except that vomiting is slightly more common with influenza B.5 Influenza A is more severe in adults, while influenza B is more common in children younger than the age of 5 years. Influenza A can move between humans, animals, and birds, while influenza B can only infect humans.6
Current surveillance data from the severely impactful 2024-2025 season demonstrate the national scope of activity. Over the course of the season (Sept. 29, 2024, through Aug. 30, 2025), 3,978,954 specimens were tested for influenza by clinical laboratories reporting to the CDC, with 489,579 (12.3%) yielding positive results. Of the positive specimens, 88.8% of cases were identified as influenza A and 11.2% as influenza B. Influenza hospitalizations remain most significant in patients aged 65 years and older, who account for 57% of all estimated hospitalizations. Pediatric patients younger than 5 years of age also experienced disproportionately high cumulative hospitalization rates (104.7 per 100,000 population) during this season.7
Additional subtypes of influenza, C and D, are less commonly associated with human disease. Influenza C produces a self-limited respiratory illness that is more common in children. Influenza D is believed to have originated in cattle and is predominantly responsible for bovine respiratory disease.
The burden of influenza on the population each year is significant, with the 2024-2025 high-severity season alone resulting in an estimated 43 million to 73 million illnesses in the United States, including 560,000 to 1,100,000 hospitalizations and 38,000 to 99,000 deaths. The widespread use of the influenza vaccine continues to be the most effective prevention method. The CDC estimates that the vaccine has prevented an estimated 9.4 million to 16 million influenza illnesses and 170,000 to 360,000 hospitalizations during the 2024-2025 season alone.7,8
Global Impact
Throughout history, several major global flu outbreaks have been documented. These outbreaks are due to the ability of viruses to change their antigenic structure rapidly. While influenza traditionally is regarded as a human disease entity, it is essential to recognize that animals, such as birds and pigs, serve as important reservoirs for viral strains. These unique properties of the virus are responsible for the significant outbreaks that have shaped human health history.
While the 1918 influenza pandemic is perhaps the best known of all outbreaks, influenza has affected human history for centuries.9 The first documented influenza outbreak may have occurred as early as 1510. While it would have been impossible for early historians to know the exact nature of the disease, this illness bore similar traits to the modern influenza virus that is well-described today. Historical accounts of a rapid-onset fever with respiratory symptoms that occurred via trade routes or in significant population centers suggest that influenza epidemics and pandemics have been present throughout human history.9
H1N1 Pandemic, 1918
The H1N1 avian flu virus had a major worldwide impact from 1918 to 1919. Historical estimates suggest that nearly 500 million people across the globe were infected, representing roughly one-third of the entire population. In the United States, the virus emerged during the spring of 1918, when military personnel were reported to have flu-like symptoms. Transmission of the virus resulted in the death of 50 million people worldwide, with roughly 675,000 deaths in the United States.10,11 In 2005, researchers successfully recreated the virus to learn more about the emergence of pandemic viruses.12
H2N2 Pandemic,1957-1958
In February 1957, the H2N2 strain of the influenza A virus resulted in the pandemic known as the “Asian flu.” Located predominantly in East Asia, the virus spread to coastal U.S. cities during the summer of 1957. Approximately 1.1 million deaths were documented worldwide, with close to 116,000 fatalities in the United States.13,14
H3N2 Pandemic, 1968
The H3N2 influenza A virus strain was first documented to reach the United States in September 1968. The estimated number of deaths was 1 million worldwide, with roughly 100,000 fatalities in the United States.15
H1N1 Pandemic, 2009
In April 2009, a novel strain of the influenza A virus, H1N1, resulted in a significant outbreak of respiratory illness. The strain emerged in Mexico and quickly spread across the United States, with more than 55 million cases worldwide. Attempts to curb infection resulted in the production of a specially formulated vaccine. The clinical impact of this virus resembled previous strains of influenza; however, increased morbidity occurred among younger adults with comorbidities. In the United States, more than 10,000 patients died from complications of the infection. The World Health Organization (WHO) declared that the pandemic was over by April 2010.16,17
H3N2 Variant Influenza, 2011
First identified in 2011, the H3N2 strain of the influenza A virus has been responsible for more than 400 cases of influenza, with the majority identified after July 2012.18 This particular strain was found to originate in swine, with the addition of the M gene from the H1N1 influenza A virus. Most patients affected reported contact with pigs before illness. Cases of this strain typically are milder and self-limited.
Avian H7N9 Influenza, 2013
The novel avian H7N9 strain was first identified in China in 2013 and has been responsible for annual epidemics during the flu season. As with the H3N2 influenza strain, there is limited evidence of direct person-to-person transmission. Most cases have been linked to poultry handling before illness. Patients with confirmed avian H7N9 flu had severe disease, with mortality rates anywhere from 27% to 36%, with pneumonia as a common complication.19,20
Epidemiology
The influenza virus carries a clinically significant health burden that tends to occur seasonally, with peak activity in the winter months. This phenomenon is associated with the antigenic shifts and antigenic drifts seen in the type A strain of the virus. Significant changes in the virus’s glycoproteins, neuraminidase and hemagglutinin, are termed antigenic shifts. These shifts are responsible for significant epidemics and pandemics that affect large populations. Minor changes in the structure of these glycoproteins result in antigenic drift, which tends to result in more localized outbreaks.21
The incidence of influenza is difficult to characterize because it is not always diagnosed and varies based on the disease burden during each season or unique epidemic. Furthermore, the incidence varies based on different age groups. The WHO estimates annual flu outbreaks cause up to 1 billion infections worldwide, with 3 million to 5 million cases of severe disease. The flu is thought to be responsible for 290,000 to 650,000 respiratory deaths annually.22 Meta-analysis of symptomatic influenza in the United States suggests an annual incidence of around 8%.23 Seasonal disease causes 290,000 to 650,000 respiratory deaths worldwide and, in the United States alone, typically results in 9.3 million to 41 million illnesses, 100,000 to 710,000 hospitalizations, and 4,900 to 51,000 deaths each year.22,24
Flu Season
While the influenza virus circulates year-round, flu season typically is when infection with influenza is the highest. In the United States, the CDC maintains annual data with weekly influenza reports available to the public.25 The incidence of respiratory secretions testing positive for influenza typically rises in mid-November and peaks in early February, as during the most recent 2024-2025 high-severity season. (See Figure 2.) The peak activity for this season (31.6% test positivity) was the highest reported in the United States since the 2015-2016 season.26 Despite this, clinicians must remember that influenza circulates continuously throughout the year and may be present at any time. Although the flu season typically occurs during the winter months in both the Northern and Southern hemispheres, flu season may occur during the year in tropical regions and may affect travelers. Similarly, sporadic outbreaks may occur on cruise ships and with airline travel.27
Figure 2. Peak Month of Flu Activity 1982-1983 Through 2024-2025 |
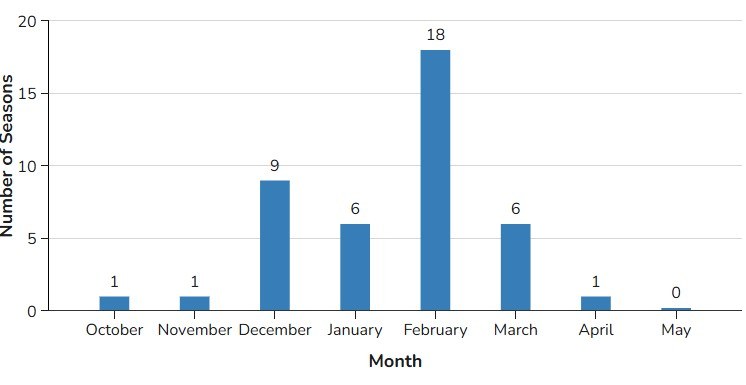 |
Source: Centers for Disease Control and Prevention. https://www.cdc.gov/flu/about/season.html?CDC_AAref_Val=https://www.cdc.gov/flu/about/season/#cdc_generic_section_1-flu-season-in-the-united-states |
Etiology
The influenza virus (genus Influenzavirus) is a negative-sense, single-strand RNA virus. Influenza A, B, C, and D have been identified, with types A and B responsible for the bulk of human pathology.15,21 The A and B viral genome contains segments of genetic material that encode viral proteins that facilitate viral replication and entry into host cells. The hemagglutinin protein allows viral entry, while the neuraminidase protein allows viral release.
Risk Factors for Severe Illness
Risk factors for severe illness or complications with influenza are similar to those for other viral pathologies that cause disease in humans. Children without significant previous exposure to the virus are at a higher risk for infection with more severe features, particularly those younger than 5 years of age.6 Because of their decreased immune system function and significant medical comorbidities, older adults aged 65 years and older are at higher risk for severe illness that often requires hospitalization.6 This population bears a major burden of the disease and its complications.28,55
Patients with neurologic or neuromuscular disorders and chronic pulmonary pathology also are more susceptible to severe infection. This risk is thought to be due to diminished respiratory muscle strength and impaired handling of respiratory secretions.29 Pregnant females have an increased risk throughout gestation and that persists through the postpartum period.30 Individuals who are extremely obese (body mass index [BMI] ≥ 40) are at higher risk of infection because of several proposed mechanisms. Reduced vaccination efficacy and increased viral replication have been described in patients with a significantly elevated BMI. Morbid obesity has been independently associated with increased risk of hospitalization and death due to influenza, even in the absence of other chronic diseases.31
Pathophysiology
Influenza virus is spread from person to person mainly via large droplet transmission that occurs during sneezing and coughing. Transmission from host to recipient occurs when both parties are within close contact with each other, typically less than six feet, since the large droplets do not remain aerosolized for significant periods of time.29,79 However, evidence supports that infectious influenza virus also can be recovered from small-particle aerosols exhaled during routine breathing and coughing, which may contribute to transmission, especially in the immediate vicinity of a patient.32
The virus enters the airways and targets epithelial cells for subsequent replication. The virus binds to the cell wall by interacting with the virus’s hemagglutinin glycoprotein and sialic acid glycoproteins on the host cell wall. Once the virus enters the cell and replicates, the neuraminidase glycoprotein helps release replicated virions. This process leads to the affected cells’ eventual apoptosis and the virus’s subsequent spread.
Infectious Course
The incubation period for influenza typically is one to four days (average two days). Viral shedding is thought to occur within 24 to 48 hours before symptom onset, although there is less of a viral burden than when the patient is symptomatic.32 Peak viral shedding has been shown to occur two days after the onset of symptoms. Longer shedding periods may occur with certain patient populations, such as children, older adults, immunocompromised patients, or those with chronic medical conditions. Viral shedding generally resolves among most adults by day 7 after symptom onset.33 However, children, particularly those younger than 5 years of age, consistently demonstrate greater peak shedding and longer durations of shedding compared to adults.34,35 In severely ill or immunocompromised patients, viral shedding can be protracted, lasting for weeks or even months.36,37
Uncomplicated influenza infection typically manifests with an acute onset of fever, headache, myalgias, and malaise. Following these initial symptoms, patients commonly experience symptoms associated with respiratory tract disease, such as cough, sore throat, and rhinorrhea. Patients with uncomplicated influenza usually recover from their illness within two to five days, although complete symptom resolution may take upward of one week or more, with cough persisting more than two to three weeks in about 15%.38
Clinical Presentation
The clinical presentation of uncomplicated influenza mimics other respiratory viral syndromes. Patients often present with the abrupt onset of symptoms within one to four days of exposure to the virus. Symptomatology can range from mild to life-threatening and can last for up to two weeks.38
The initial symptoms after infection typically include acute onset of high fevers, intense myalgias, headaches, and malaise. As the infection progresses, patients exhibit respiratory tract symptoms, such as nasal congestion, rhinorrhea, sore throat, and a nonproductive cough. The presence of gastrointestinal symptoms, such as vomiting and diarrhea, is seen in a minority of adult patients but is far more common in pediatric patients.38
The physical examination often is remarkable for a fever with the presence of posterior cervical adenopathy and erythematous mucous membranes of the nasopharyngeal passages. The oropharynx may appear hyperemic, and the lung examination can vary from a normal pulmonary exam to rales secondary to superimposed pneumonia. Tachycardia may present as a response to the febrile state or dehydration secondary to decreased oral intake. Children may exhibit erythematous tympanic membranes suggesting acute otitis media.
Patients at the extremes of age may present atypically. Older adults (age ≥ 65 years) often manifest few classic systemic symptoms. Instead, the primary presentation may be a simple decline in functional status, altered mental status, or an acute exacerbation of underlying chronic medical comorbidities such as heart failure and chronic pulmonary disease. Careful consideration should be applied when evaluating this subset of patients since diagnosis is not always straightforward.38
Differential Diagnosis
Influenza presents similarly to other respiratory viruses. A thorough history and physical examination by the emergency physician (EP) can help guide the evaluation of patients for potential etiologies. Upper respiratory infections caused by other viral agents, such as adenovirus, rhinovirus, and RSV, present similarly to influenza.
Overlapping symptoms, such as rhinorrhea, myalgias, and cough, can predominate the clinical picture. Other infectious pathologies, such as meningitis, pneumonia, pyelonephritis, and sepsis, should be considered when evaluating flu-like symptoms. A thorough travel and exposure history should be pursued to screen for other etiologies, such as dengue fever or Ebola. This broad differential can make diagnosis challenging for the EP.
COVID-19 (SARS-CoV-2) was first identified in 2019 and went on to become a global pandemic that has resulted in more than 7.0 million deaths worldwide.39 This virus is similar to influenza since both are spread primarily through the respiratory route. History and physical exam alone cannot determine viral etiology. Table 1 depicts common similarities and differences between these two viral syndromes.
Interestingly, between October 2020 and May 2021, during the COVID-19 pandemic, influenza activity in the United States was the lowest since data became available in 1977. Only 0.05% of the 1 million samples tested were influenza-positive. This marked reduction in disease burden has been attributed to decreased travel, increased mask usage, and focus on physical distancing.40
Table 1. Comparing COVID-19 and Influenza |
Influenza |
|
COVID-19 |
|
Source: Centers for Disease Control and Prevention. Similarities and differences between flu and COVID-19. https://www.cdc.gov/flu/about/flu-vs-covid19.html. Last reviewed Sept. 17, 2024 |
Diagnosis and Testing
Influenza often can be diagnosed presumptively based on a thorough history and physical examination without the need for routine diagnostic testing during an established local outbreak or epidemic period.17 The abrupt onset of a febrile respiratory illness with systemic symptoms, such as myalgias and headaches, during peak months can guide clinicians toward a presumptive diagnosis.
Laboratory testing is available and should be reserved for instances in which confirmatory testing will affect patient care. Molecular assays are the preferred specimen type across all age groups.44 In infants and young children, nasal aspirates and swabs are the preferred specimens for testing. Older children and adults should provide specimens from the nasopharynx. In mechanically ventilated patients, endotracheal aspirates or bronchiolar lavage fluid should be obtained for evaluation of the lower respiratory tract.
Suggested uses for rapid diagnostic testing include all hospitalized patients, patients in whom there is diagnostic uncertainty, patients with significant medical comorbidities, and documentation for institutional purposes. In addition, testing for both influenza and COVID-19 is recommended when the results will lead to a change in management, such as in patients at risk for progression to severe disease.42 Individual providers should contact their laboratory for detailed information regarding the performance of the specific diagnostic test used at their institution.
Rapid Antigen Testing
Rapid antigen testing (rapid influenza diagnostic test [RIDT]) can identify viral nucleoprotein antigens in respiratory specimens. Data suggest that this testing method carries a pooled sensitivity of around 62% and specificity of 98%.43 Although these tests can produce results in as quick as 15 minutes, their low sensitivity often necessitates confirmatory molecular testing if the result is negative in a high-prevalence setting.41
Polymerase Chain Reaction
The polymerase chain reaction (PCR) method of diagnosis, including nucleic acid amplification tests (NAAT), is considered the gold standard because of its superior sensitivity and specificity, which typically approach 100%. The drawback that PCR assays are burdensome and take upward of eight hours is no longer universally true. Many newer molecular assays are Food and Drug Administration (FDA)-cleared for point-of-care use and can provide highly accurate results in the emergency department (ED) setting within 15 to 30 minutes, making them the preferred diagnostic method.44
Viral Culture
Viral culture, while historically viewed as the definitive gold standard, has a prolonged turnaround time of 48-72 hours. Therefore, it is obsolete for initial clinical management in the emergency setting and now is used primarily by public health laboratories for surveillance purposes, including virus isolation and further genetic and antigenic characterization.44
Complications
Patients with influenza may progress to develop more severe complications, which are broadly categorized as pulmonary and extrapulmonary. The most frequent serious complications involve the respiratory tract, specifically primary influenza pneumonia and secondary bacterial pneumonia.45 Primary influenza pneumonia is a severe, direct result of viral infection that typically occurs early in the illness and can progress rapidly to respiratory distress.47 More commonly, patients develop secondary bacterial pneumonia, which often presents later, around the end of the first or beginning of the second week, following a period of initial improvement.45 The incidence of pneumonia as a complication often is higher among those with preexisting risk factors, and tools are being developed to help predict the risk of progression to pneumonia and death.47 While Streptococcus pneumoniae remains the most common bacterial culprit, clinicians also must recognize the increasing prevalence of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA), an agent associated with rapid clinical deterioration and high mortality.45,48 As evidence of this burden, one study found that 39.5% of hospitalized adults with influenza in a large cohort developed secondary bacterial pneumonia.47 The presence of pneumonia itself is an independent risk factor for cardiac complications.58
Beyond the respiratory system, influenza is a systemic illness that can trigger a range of serious extrapulmonary complications, often mediated by widespread inflammation and a dysregulated host immune response.50,51 The infection is strongly and consistently associated with a heightened risk of major cardiovascular events; specifically, a laboratory-confirmed influenza infection is associated with an elevated incidence of acute myocardial infarction (AMI), with the risk being up to six-fold higher in the week following the infection.54 Influenza also can lead to direct cardiac complications, including myocarditis (inflammation of the heart muscle), pericarditis, and the exacerbation of preexisting heart failure.50 Furthermore, influenza can affect the central nervous system, resulting in neurologic complications such as encephalitis and encephalopathy.56 In a review of pediatric influenza-associated deaths, influenza-associated encephalopathy or encephalitis (IAE) was identified as a significant cause of mortality, with the most severe forms being associated with high rates of long-term disability and death.56 Less common but still serious systemic issues include myositis and rhabdomyolysis — muscle breakdown that can lead to acute kidney injury — which are particularly recognized with influenza A and H1N1 strains.46,57 Finally, other severe systemic issues include sepsis and toxic shock syndrome, with the latter following influenza, carrying a high reported mortality rate.56
Management
The mainstay of management for most adults and children infected with the influenza virus remains supportive care since the disease state usually is self-limited. Otherwise, healthy patients without significant comorbidities may achieve symptomatic relief with over-the-counter medications and adequate oral hydration.
When initiated promptly, antiviral therapy has been shown to play a role in shortening the duration of influenza symptoms. The greatest benefit of these medications has been demonstrated when given to febrile patients as soon as possible, ideally within the first 48 hours of symptom onset.59
The two major classes of antiviral medications for influenza are neuraminidase inhibitors (oral oseltamivir, inhaled zanamivir, and intravenous peramivir) and a cap-dependent endonuclease inhibitor (oral baloxavir marboxil).59 Adamantanes (oral amantadine and rimantadine) are not recommended for use because of widespread resistance to circulating influenza A strains.60 Consequently, neuraminidase inhibitors and baloxavir predominate as the antiviral therapy of choice when treating suspected or confirmed cases of influenza in most patients.
Current clinical guidelines from the CDC and the Infectious Diseases Society of America (IDSA) recommend initiation of antiviral therapy as soon as possible with confirmed or suspected cases of influenza in patients with severe illness, hospitalized patients, and patients at high risk of complications (irrespective of symptom duration).59 The decision to administer therapy should not be delayed or depend on the results of diagnostic testing.
Conversely, healthy adults and children with presumed or confirmed influenza may be treated electively as outpatients with neuraminidase inhibitors. Studies in these populations demonstrated a small decrease in duration of illness in adults by approximately one day.61 Shared decision-making with the patient on a case-by-case basis can help guide the decision to initiate medical therapy.
Specific Antiviral Agents
Oseltamivir
Oseltamivir (U.S. brand name: Tamiflu) currently is one of the most frequently prescribed medications used in the management of influenza.60 The typical dosage regimen for oseltamivir is described in Table 2. Treatment should be initiated within 48 hours of the onset of illness and continued for five days.62 Adult patients with a creatinine clearance (CrCl) of 30 mL/min to 60 mL/min should have their dose adjusted to 30 mg twice daily. For patients with severe renal impairment (CrCl < 30 mL/min), the recommended dose is 30 mg once daily.62 While the drug was formerly considered pregnancy class C, the American College of Obstetricians and Gynecologists (ACOG) and the CDC recommend presumptive treatment with antiviral medication during pregnancy.59,74 Common side effects include headache, nausea, and vomiting.62
Table 2. Oseltamivir Dosing for Oral Treatment67 |
Adults (Normal Renal Function) |
|
Adults with Moderate Renal Impairment (CrCl = 30 mL/min to 60 mL/min) |
|
Adults with Severe Renal Impairment (CrCl = 10 mL/min to 30 mL/min) |
Dose: 30 mg once daily Duration: Five days |
Children (1-12 years of age) |
|
Infants (2 weeks to younger than 1 year of age) |
|
CrCl: creatinine clearance |
Baloxavir Marboxil
Baloxavir marboxil (U.S. brand name: Xofluza) is an oral cap-dependent endonuclease inhibitor approved for treatment of acute, uncomplicated influenza in people 5 years of age and older.64-66 It works by blocking messenger RNA (mRNA) synthesis of endonucleases responsible for viral proliferation.64 Results from a randomized controlled trial comparing baloxavir marboxil to oseltamivir demonstrated superiority in the reduction of viral load one day after initiation of pharmacotherapy for patients receiving baloxavir marboxil.69 The introduction of baloxavir was noted to be a significant step forward in influenza treatment.68 One randomized trial showed that baloxavir had a shorter median time to resolution of symptoms when compared to oseltamivir or placebo.69 Baloxavir generally is not recommended for use in hospitalized, pregnant, or breastfeeding patients because of limited data.60
Treatment and Prophylaxis Guidelines
Patients who require hospitalization or who are deemed to be at high risk for influenza complications should be treated with a neuraminidase inhibitor (preferably oseltamivir or intravenous peramivir) regardless of duration of symptoms. These risk factors include age older than 65 years, pregnancy, and chronic comorbid medical conditions. Initiation of therapy should not be delayed while waiting for diagnostic or confirmatory testing.70
Chemoprophylaxis for patients exposed to suspected or confirmed flu cases remains a controversial topic. In general, guidelines discourage routine use of chemoprophylaxis with antivirals. Patients exposed to influenza who are at high risk for complications and cannot be vaccinated because of contraindications should be considered as candidates. For appropriate patients older than 5 years of age with a known exposure, post-exposure prophylaxis can be administered with oseltamivir (treatment dose administered once a day for seven days) or a single dose of baloxavir marboxil.67
Antiviral resistance is constantly being monitored by the CDC. During the 2024-2025 flu season, almost all circulating influenza viruses tested were susceptible to the commonly prescribed oral agents and baloxavir, with only a small number of viruses demonstrating reduced susceptibility. The CDC maintains that current guidance on medication management for influenza remains appropriate.71
COVID Therapeutics
While the clinical syndrome of COVID and influenza may overlap, treatment strategies rely on different medication agents. Paxlovid (nirmatrelvir with ritonavir) is an antiviral agent approved in the United States for adults and children aged 12 years and older. This oral medication should be started as soon as possible and within five days of symptom onset for patients at high risk of progressing to severe disease. Caution is advised when prescribed, since many drug-drug interactions may preclude its use. Veklury (remdesivir) is an intravenous antiviral medication approved for COVID in adults and children. This medication must be administered for three consecutive days in the outpatient setting, typically at a healthcare facility. For hospitalized patients, the recommended course is five days.72 Similar to Paxlovid, this medication should be administered as soon as possible, within seven days of symptom onset.
Prevention
Vaccination remains the cornerstone for primary flu prevention. Because annual influenza vaccines typically are 40% to 60% effective in reducing seasonal infections, there remains significant potential for disease despite vaccination.75
Given the high rates of new strains that develop from significant antigenic variation, vaccines are reformulated annually to match expected circulating strains. These formulations generally are developed six months before flu season based on surveillance data from the previous year.71
The seasonal influenza vaccine is recommended for yearly administration in patients 6 months of age and older who do not have any known contraindications for vaccination.75 This includes pregnant women (regardless of gestational age) and women who are breastfeeding.74 (See Table 3.)
Table 3. Influenza Vaccines |
Standard Precaution (All Vaccines): Moderate or severe acute illness. History of severe allergic reaction. History of Guillain-Barré syndrome (GBS) within six weeks of prior vaccine. |
IIV (Standard-Dose Trivalent) |
|
ccIIV (Cell-Culture) |
|
Flublok (Recombinant) |
|
Fluzone High-Dose |
|
Fluad |
|
FluMist |
|
Source: Centers for Disease Control and Prevention. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2025–2026 Influenza Season. MMWR Recomm Rep. 2025;74(RR-2). |
United States vaccine supplies for the 2025-2026 flu season are projected to reach 154 million doses. All standard-dose vaccines are quadrivalent for the current flu season, meaning they will protect against two influenza A and two influenza B virus strains.75
Recently, researchers have been working to establish universal vaccination. This vaccine would function to elicit the creation of protective antibodies in vaccinated patients against well-conserved viral proteins.76,77
Like with influenza, the FDA has authorized or licensed vaccines designed to prevent COVID. The CDC currently recommends an updated COVID-19 vaccine dose for most adults aged 65 years and older and those at high-risk for complications. COVID-19 vaccination recommendations for individuals younger than age 65 years are increasingly determined by individual decision-making based on risk factors.78 The CDC continues to maintain and track data to understand vaccine effectiveness.
Disposition
The vast majority of patients diagnosed with influenza from the ED may be discharged safely home with strong return precautions. Patients discharged from the ED should follow up with a primary care provider for reevaluation in two days for reexamination and monitoring of the patient’s clinical course. Before discharge, patients should demonstrate an ability to ambulate steadily and tolerate oral intake without any difficulty. Additionally, vital signs should be reevaluated prior to discharge planning for any hypoxemia, persistent tachycardia, or tachypnea. The febrile state is expected with the disease process, and clinicians should consider the effects of administration of antipyretics when evaluating the significance of fever in the ED. It is important to note that fever and dehydration can drive tachycardia; however, if the patient remains persistently tachycardic despite therapy, the provider should consider possible complications like myocarditis or superimposed bacterial infection/sepsis.
Discharge instructions should educate patients on signs and symptoms that should prompt a patient to seek immediate medical attention. Persistent fevers, inability to tolerate oral intake, confusion, or changes in mental status should be reinforced clearly as reasons to return to the ED.
On discharge, patients diagnosed with influenza should be educated on hand washing, respiratory hygiene, and cough etiquette to decrease the risk of viral spread.
Supportive care with antipyretics, rest, and hydration are the mainstays of outpatient therapy. Treatment with an antiviral agent may be initiated without diagnostic testing in the appropriate clinical setting. Patients should be counseled regarding the risks and benefits of medical therapy before initiation with a neuraminidase inhibitor.
Observation
Certain patients may benefit from observation in the hospital or ED depending on institutional practices. Patients should be placed on droplet precautions to limit the spread of viral illness within the healthcare facility.79 The observation setting may be a useful disposition for patients who may benefit from serial cardiopulmonary examinations and/or intravenous hydration secondary to clinically significant dehydration. Patients at the extremes of age without significant medical comorbidities may benefit from this extended period of medical observation.
Prior to discharge, patients should be reevaluated for symptomatic control and ability to tolerate oral intake. If a patient’s clinical response to symptomatic therapy fails to improve, strong consideration should be given for admission to the hospital for further management in the inpatient setting.
Hospitalization
From 2011-2019, the estimated number of patients hospitalized annually due to influenza in the United States ranged from 140,000 to 810,000.80 Estimates from the 2024-2025 season indicate that this number has grown to 560,000 to 1,100,000 individuals.7 The decision to admit a patient to the hospital for flu can be particularly challenging, since no well-validated scoring system exists to guide disposition. This decision should be based on clinical judgment along with assessment of the patient’s risk factors and disease burden.
A subset of patients presenting to the ED should be considered strongly for hospital admission due to concerns about decompensation from the viral illness. Adults aged 65 years or older, pregnant women, children younger than 5 years of age, and individuals with comorbid conditions should be considered for admission. These high-risk factors warrant prompt initiation of antiviral therapy and are the primary driver for hospitalization consideration. (See Table 4.) Additionally, patients who have been previously evaluated by a medical provider and have not improved with outpatient management should be considered for admission
Table 4. Comorbid Conditions That Increase the Risk of Severe Influenza Complications | |
Category | Conditions/Patient Factors |
Pulmonary | Chronic pulmonary disease (e.g., asthma, COPD, cystic fibrosis, bronchopulmonary dysplasia) |
Cardiovascular | Cardiovascular disease (excluding isolated hypertension) |
Metabolic/Endocrine | Diabetes mellitus and other chronic metabolic disorders |
Renal/Hepatic | Chronic renal disease, chronic liver disease |
Neurologic/Neuromuscular | Neurologic and neurodevelopmental conditions (e.g., stroke, cerebral palsy, epilepsy, neuromuscular disorders that impair handling of respiratory secretions) |
Hematologic | Chronic hematologic disorders (e.g., sickle cell disease) |
Immunosuppression | Immunosuppression due to any cause (e.g., HIV infection, cancer, transplant, or medications) |
COPD: chronic obstructive pulmonary disease; HIV: human immunodeficiency virus Source: Centers for Disease Control and Prevention. People at increased risk for flu complications. https://www.cdc.gov/flu/highrisk/index.htm. Last reviewed Sept. 11, 2024. | |
Patients with influenza may deteriorate to acute respiratory distress syndrome (ARDS), requiring possible intubation and intensive care for hypoxemic respiratory failure. Patients who develop ARDS may require extracorporeal membrane oxygenation (ECMO) as a bridge therapy during the acute phase of their illness.45 The EP should proceed cautiously with patients who present with hypoxemia because these patients may progress to respiratory failure.
Patients who are deemed to be at high risk for worsening of clinical conditions because of comorbidities or changes in mental status should be screened for intensive care admission when available. Additionally, patients experiencing complications from influenza, such as myocarditis, typically require hospital admission. Consultation with a pulmonologist or infectious disease specialist can be obtained in the inpatient setting, depending on the patient’s clinical course or past medical history, as applicable.
Conclusion
Influenza outbreaks occur each year, with their nature and extent largely determined by the virus’s glycoprotein structure and antigenic properties. These outbreaks typically occur during the winter months and can confer high morbidity to the general patient population. Increased mortality rates are seen in children younger than 5 years of age, older adults, and those with chronic comorbid medical conditions.
During the winter months, EPs should maintain a high suspicion for influenza in all patients presenting with an acute febrile respiratory illness. While the differential diagnosis is broad, the history and physical examination can guide the EP toward a presumptive diagnosis without the need for additional testing. Molecular assays are the preferred laboratory testing method and should be reserved for those patients in whom the diagnosis may change the patient’s clinical management.
Treatment is indicated for severely ill patients or those at risk for complications. Initiation of antiviral treatment should be as soon as possible, ideally within 48 hours of symptom onset, while the vast majority of otherwise healthy patients can be managed with supportive care only. Complicated cases of influenza may require hospitalization and treatment with antiviral therapy regardless of the time since symptom duration.
Prevention against the influenza virus is achieved primarily through the annual influenza vaccine. This vaccine attempts to protect patients from the most commonly circulating strains of the virus. This is accomplished by obtaining routine surveillance data about viral characteristics during each flu season.
Emerging therapy, including single-dose antiviral medications and universal vaccination, may shape the rapidly evolving nature of the influenza virus and its burden on human health.
Michael Ullo, MD, MHCI, FACEP, is Vice Chair, Quality & Patient Safety, Department of Emergency Medicine, Hackensack University Medical Center, Hackensack, NJ.
Gregory Sugalski, MD, MBA, is Regional Chairman, Department of Emergency Medicine, Hackensack University Medical Center, Hackensack, NJ.
References
1. Centers for Disease Control and Prevention. Influenza activity in the United States during the 2024-25 season and composition of the 2025-26 influenza vaccine. Sept. 26, 2025. https://www.cdc.gov/flu/whats-new/2025-2026-influenza-activity.html
2. Reinhart K, Huang S, Kniss K, Reed C, Budd A. Influenza-associated pediatric deaths — United States, 2024-25 influenza season. MMWR Morb Mortal Wkly Rep. 2025;74:565-569.
3. Centers for Disease Control and Prevention. 2025-2026 flu season. Aug. 6, 2025. https://www.cdc.gov/flu/season/2025-2026.html
4. Centers for Disease Control and Prevention. FluView: U.S. influenza surveillance report. https://www.cdc.gov/fluview/index.html
5. Karolyi M, Pawelka E, Daller S, et al. Is there a clinical difference between influenza A and B virus infections in hospitalized patients? Results after routine polymerase chain reaction point-of-care testing in the emergency room from 2017/2018. Wien Klin Wochenschr. 2019;131:362-368.
6. Centers for Disease Control and Prevention. Types of influenza viruses. Sept. 26, 2025. https://www.cdc.gov/flu/about/viruses-types.html?CDC_AAref_Val=https://www.cdc.gov/flu/about/viruses/types.htm
7. Centers for Disease Control and Prevention. Influenza activity in the United States during the 2024-25 season and composition of the 2025-26 influenza vaccine. Sept. 26, 2025. https://www.cdc.gov/flu/whats-new/2025-2026-influenza-activity.html
8. Reed C, Chaves SS, Daily Kirley P, et al. Estimating influenza disease burden from population-based surveillance data in the United States. PLoS One. 2015;10:e0118369.
9. Morens DM, Taubenberger JK, Folkers GK, Fauci AS. Pandemic influenza’s 500th anniversary. Clin Infect Dis. 2010;51:1442-1444.
10. Jester B, Uyeki T, Jernigan D. Readiness for responding to a severe pandemic 100 years after 1918. Am J Epidemiol. 2018;187:2596-2602.
11. Belser JA, Tumpey TM. The 1918 flu, 100 years later. Science. 2018;359:255.
12. Tumpey TM, Basler CF, Aguilar PV, et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;310(5745):77-80.
13. Viboud C, Simonsen L, Fuentes R, et al. Global mortality impact of the 1957-1959 influenza pandemic. J Infect Dis. 2016;213:738-745.
14. Langmuir AD. Epidemiology of Asian influenza. With special emphasis on the United States. Am Rev Respir Dis. 1961;83:2-14.
15. Glezen WP. Emerging infections: Pandemic influenza. Epidemiol Rev. 1996;18:64-76.
16. Reed C, Angulo FJ, Swerdlow DL, et al. Estimates of the prevalence of pandemic (H1N1) 2009, United States, April-July 2009. Emerg Infect Dis. 2009;15:2004-2007.
17. Walls RM, Hockberger RS, Gausche-Hill M. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Elsevier; 2018.
18. Schicker RS, Rossow J, Eckel S, et al. Outbreak of influenza A(H3N2) variant virus infections among persons attending agricultural fairs housing infected swine — Michigan and Ohio, July-August 2016. MMWR Morb Mortal Wkly Rep. 2016;65:1157-1100.
19. Gao R, Cao B, Hu Y, et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med. 2013;368:1888-1897.
20. Yu H, Cowling BJ, Feng L, et al. Human infection with avian influenza A H7N9 virus: An assessment of clinical severity. Lancet. 2013;382:138-145.
21. Jain R, Sharma H, Pena L, et al. Influenza virus: Genomic insights, evolution, and its clinical presentation. Microb Pathog. 2025;205:107671.
22. World Health Organization. The burden of influenza. Last reviewed March 30, 2024. www.who.int/news-room/feature-stories/detail/the-burden-of-influenza
23. Tokars JI, Olsen SJ, Reed C. Seasonal incidence of symptomatic influenza in the United States. Clin Infect Dis. 2018;66(10):1511-1518.
24. Naquin A, O’Halloran A, Ujamaa D, et al. Laboratory-confirmed influenza-associated hospitalizations among children and adults — Influenza Hospitalization Surveillance Network, United States, 2010-2023. MMWR Surveill Summ. 2024;73(6):1-18.
25. Centers for Disease Control and Prevention. FluView: Current week’s U.S. influenza surveillance report. Sept. 6, 2025. https://www.cdc.gov/fluview/surveillance/week-38.html
26. Centers for Disease Control and Prevention. Influenza activity in the United States during the 2024–25 season and composition of the 2025–26 influenza vaccine. Last reviewed Sept. 26, 2025. https://www.cdc.gov/flu/whats-new/2025-2026-influenza-activity.html
27. Brownstein JS, Wolfe CJ, Mandl KD. Empirical evidence for the effect of airline travel on inter-regional influenza spread in the United States. PLoS Med. 2006;3:e401.
28. Stotts C, Corrales-Medina VF, Rayner KJ. Pneumonia-induced inflammation, resolution and cardiovascular disease: Causes, consequences and clinical opportunities. Circ Res. 2023;132(10):751-774.
29. Centers for Disease Control and Prevention. People at increased risk for flu complications. Sept. 11, 2024. https://www.cdc.gov/flu/highrisk/
30. World Health Organization. Influenza (seasonal) fact sheet. Last reviewed Feb. 28, 2025. https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal)
31. Morgan OW, Bramley A, Fowlkes A, et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease. PLoS One. 2010;5(3):e9694.
32. Yan J, Grantham M, Pantelic J, et al. Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc Natl Acad Sci U S A. 2018;115(5):1081-1086.
33. Stone EC, Okasako-Schmucker DL, Taliano J, et al. Risk period for transmission of SARS-CoV-2 and seasonal influenza: A rapid review. Infect Control Hosp Epidemiol. 2025;46(3):1-9.
34. Carrat F, Vergu E, Ferguson NM, et al. Time lines of infection and disease in human influenza: A review of volunteer challenge studies. Am J Epidemiol. 2008;167:775-785.
35. Leekha S, Zitterkopf NL, Espy MJ, et al. Duration of influenza A virus shedding in hospitalized patients and implications for infection control. Infect Control Hosp Epidemiol. 2007;28:1071-1076.
36. Klimov AI, Rocha E, Hayden FG, et al. Prolonged shedding of amantadine-resistant influenzae A viruses by immunodeficient patients: Detection by polymerase chain reaction-restriction analysis. J Infect Dis. 1995;172:1352-1355.
37. Loeb M, Singh PK, Fox J, et al. Longitudinal study of influenza molecular viral shedding in Hutterite communities. J Infect Dis. 2012;206:1078-1084.
38. Centers for Disease Control and Prevention. Clinical signs and symptoms of influenza. Last reviewed Aug. 8, 2024. https://www.cdc.gov/flu/hcp/clinical-signs/
39. World Health Organization. WHO coronavirus (COVID-19) dashboard. Sept. 28, 2025. https://data.who.int/dashboards/covid19/cases?n=c
40. Olsen SJ, Winn AK, Budd AP, et al. Changes in influenza and other respiratory virus activity during the COVID-19 pandemic — United States, 2020-2021. MMWR Morb Mortal Wkly Rep. 2021;70(33):1013-1019.
41. Centers for Disease Control and Prevention. Information for clinicians on rapid diagnostic testing for influenza. Last updated Sept, 17, 2024. https://www.cdc.gov/flu/hcp/testing-methods/rapidclin.html
42. Centers for Disease Control and Prevention. Testing and respiratory viruses. Last updated Aug. 18, 2025. https://www.cdc.gov/respiratory-viruses/prevention/testing.html
43. Chartrand C, Leeflang MM, Minion J, et al. Accuracy of rapid influenza diagnostic tests: A meta-analysis. Ann Intern Med. 2012;156(7):500-511.
44. Centers for Disease Control and Prevention. Information on rapid molecular assays, RT-PCR, and other molecular asays for diagnosis of influenza virus infection. Last updated Oct. 21, 2019. https://www.cdc.gov/flu/hcp/testing-methods/molecular-assays.html
45. Kalil AC, Thomas PG. Influenza virus-related critical illness: Pathophysiology and epidemiology. Crit Care. 2019;23(1):258.
46. MacIntyre CR, Chughtai AA, Barnes M, et al. The role of pneumonia and secondary bacterial infection in fatal and serious outcomes of pandemic influenza a(H1N1)pdm09. BMC Infect Dis. 2018;18:637.
47. Miyashita K, Nakatani E, Hozumi H, et al. Risk factors for pneumonia and death in adult patients with seasonal influenza and establishment of prediction scores: A population-based study. Open Forum Infect Dis. 2021;8(3):ofab068.
48. Li W, Di Z, Lv X, et al. Characteristics of adults with influenza A virus pneumonia and co-infections identified by mNGS in Jilin, China during 2024-2025. Front Cell Infect Microbiol. 2025;15:1662422.
49. Warren-Gash C, Hayward AC, Hemingway H, et al. Influenza infection and risk of acute myocardial infarction in England and Wales: A CALIBER self-controlled case series study. J Infect Dis. 2012;206(12):1652-1659.
50. Kalantar Neyestanaki MH, Kalantar Neyestanaki M. Influenza and its cardiovascular complications: A comprehensive review. Acta Angiol. 2024;30(3):69-78.
51. Sanchis J, et al. Increased risk of acute MI after influenza virus infection. PACE-CME. 2024.
52. Sudnik P, Walsh EE, Branche AR, et al. Comprehensive analysis of cardiovascular events and risk factors in patients hospitalized with respiratory syncytial virus. Clin Infect Dis. 2025;ciaf310.
53. Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378(4):345-353.
54. Barnes M, Heywood AE, Mahimbo A, et al. Acute myocardial infarction and influenza: A meta-analysis of case–control studies. Heart. 2015;101(21):1738-1741.
55. Conrad A, Valour F, Vanhems P. Burden of influenza in the elderly: A narrative review. Curr Opin Infect Dis. 2023;36(4):296-302.
56. Wong KK, Jain S, Blanton L, et al. Influenza-associated pediatric deaths in the United States, 2004-2012. Pediatrics. 2013;132(5):796-804.
57. Geladari E, Papademetriou V, Moore H, Lu D. A case of influenza type A myocarditis that presents with ST elevation MI, cardiogenic shock, acute renal failure, and rhabdomyolysis and with rapid recovery after treatment with oseltamivir and intra-aortic balloon pump support. Cardiovasc Revasc Med. 2018;19(1 Pt A):37-42.
58. Fadila MF, Wool KJ. Rhabdomyolysis secondary to influenza a infection: A case report and review of the literature. N Am J Med Sci. 2015;7(3):122-124.
59. Centers for Disease Control and Prevention. Treating flu with antiviral drugs. Last reviewed Sept. 11, 2024. https://www.cdc.gov/flu/treatment/antiviral-drugs.html
60. [No authors listed]. Antiviral drugs for seasonal influenza for 2024–2025. Med Lett Drugs Ther. 2024;66(1717):193–200.
61. Jefferson T, Demicheli V, Deeks J, Rivetti D. Neuraminidase inhibitors for preventing and treating influenza in healthy adults. Cochrane Database Syst Rev. 2000;(2)CD001265.
62. Genentech. Tamiflu prescribing information. FDA Approved Labeling. Last revised 8/2019. https://www.gene.com/download/pdf/tamiflu_prescribing.pdf
63. [No authors listed]. ACOG committee opinion no. 732: Influenza vaccination during pregnancy. Obstet Gynecol. 2018;131(4):e109–e114.
64. Genentech. Xofluza prescribing information. FDA Approved Labeling. Last revised 10/2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/210854s000lbl.pdf
65. U.S. Food and Drug Administration. FDA approves new drug to treat influenza [news release]. Oct. 24, 2018. https://wayback.archive-it.org/7993/20201219235001/https://www.fda.gov/news-events/press-announcements/fda-approves-new-drug-treat-influenza
66. Heo Y-A. Baloxavir: First global approval. Drugs. 2018;78:693-697.
67. Centers for Disease Control and Prevention. Influenza antiviral medications: Summary for clinicians. Last reviewed Dec. 8, 2023. https://www.cdc.gov/flu/hcp/antivirals/summary-clinicians.html
68. Uyeki TM. A step forward in the treatment of influenza. N Engl J Med. 2018;379:975-977.
69. Hayden FG, Sugaya N, Hirotsu N, et al. Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med. 2018;379(10):913-923.
70. Fiore AE, Fry A, Shay D, et al. Antiviral agents for the treatment and chemoprophylaxis of influenza — recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2011;60:1-24.
71. Centers for Disease Control and Prevention. Influenza activity in the United States during the 2024-25 season and composition of the 2025-26 influenza vaccine. Last reviewed Sept. 26, 2025. https://www.cdc.gov/flu/whats-new/2025-2026-influenza-activity.html
72. Infectious Diseases Society of America. IDSA guidelines on the treatment and management of patients with COVID-19. Last updated May 30, 2025. https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/
73. Skerrett C. Flu season 2025: When is the best time to get a flu shot? Healthline. Last updated Sept. 19, 2025. https://www.healthline.com/health-news/flu-season-2025-influenza-vaccine
74. [No authors listed]. ACOG committee opinion no. 732: influenza vaccination during pregnancy. Obstet Gynecol. 2018;131(4):e109–e114.
75. Centers for Disease Control and Prevention. 2025-2026 flu season. Last reviewed Sept. 26, 2025. https://www.cdc.gov/flu/season/2025-2026.html
76. Lambert LC, Fauci AS. Influenza vaccines for the future. N Engl J Med. 2010;363:2036-2044.
77. Erbelding EJ, Post DJ, Stemmy EJ, et al. A universal influenza vaccine: The strategic plan for the National Institute of Allergy and Infectious Diseases. J Infect Dis. 2018;218:347-354.
78. U.S. Department of Health & Human Services. ACIP recommends COVID-19 immunization based on individual decision-making. HHS Press Release. Issued Sept. 19, 2025. https://www.hhs.gov/press-room/acip-recommends-covid19-vaccination-individual-decision-making.html
79. Centers for Disease Control and Prevention. Infection prevention and control strategies for seasonal influenza in healthcare healthcare settings. Last reviewed April 28, 2025. https://www.cdc.gov/flu/hcp/infection-control/healthcare-settings.html
80. Naquin A, O’Halloran A, Ujamaa D, et al. Laboratory-confirmed influenza-associated hospitalizations among children and adults — Influenza Hospitalization Surveillance Network, United States, 2010–2023. MMWR Surveill Summ. 2024;73(6):1-18.