
Pediatric Airway Management: Difficult Airways
July 1, 2025
By Alexandra Armato, MD, and Daniel Migliaccio, MD, FPD, FAAEM
Executive Summary
- Features that suggest that bag-mask ventilation may be difficult are facial anomalies caused by trauma or congenital abnormalities, limited neck mobility, obesity, obstructive lung disease, upper airway swelling, and tracheal narrowing.
- External characteristics of the patient that suggest that the proceduralist may have a difficult time with obtaining a laryngoscopic view or intubating include limited mouth opening, short and inflexible neck, large tongue, palate abnormality, and abnormally long or short thyromental distance. Copious amounts of oral blood or secretions may block the laryngoscopic view.
- “Red-flag” signs of severe to complete airway obstruction include sniffing or tripod position, drowsiness, altered mental status, markedly reduced or no air movement, severely increased work of breathing, and silent gagging or coughing.
- The first step of management of laryngospasm is removal of any triggering stimulation followed by performance of a vigorous jaw thrust maneuver to lift the tongue off the pharyngeal wall and lift the supraglottic tissues from the false vocal cords. The patient should then receive continuous positive airway pressure with 100% oxygen.
- Two-person bag-mask ventilation is a ventilation technique that requires two rescuers. One person uses the “E-C” technique with both hands while another person squeezes the bag. The two-person technique has been shown to provide a better seal on the mask and provide a higher tidal volume to the patient with each squeeze.
- Video laryngoscopy has become used more frequently as the standard of care for the first attempt of pediatric intubations. Research has shown increased first-attempt success rates and reduced airway trauma when compared to direct laryngoscopy. Additionally, video laryngoscopy has been shown to have lower rates of severe hypoxia and desaturation events.
- Because of the small cricothyroid membrane and increased risk of laryngeal injury, open surgical cricothyrotomy is contraindicated in children younger than 10 years of age. Instead, children younger than 10 to 12 years of age should undergo needle cricothyrotomy in “cannot intubate, cannot ventilate” scenarios.
One of the most critical aspects of pediatric emergency medicine is handling a critical airway in a child. The authors provide comprehensive guidance on preparation, recognition and management to achieve success in this challenging situation.
— Ann M. Dietrich, MD, FAAP, FACEP, Editor
Introduction
Effective management of a difficult pediatric airway is a critical aspect of pediatric emergency medicine. Difficult airways present a complex medical challenge in patients with anticipated difficulty with bag-mask ventilation, laryngoscopy, or intubation of the trachea.1 Being prepared with an understanding of characteristics of a difficult airway allows providers to develop a plan to address airway issues that may arise.
Difficult Pediatric Airway Evaluation
Airways that are difficult to ventilate with bag-mask ventilation and airways that are difficult to intubate both are classified as difficult airways. Difficult airways for tracheal intubation can be further defined as those for which more than two attempts at intubation with the same laryngoscopic blade are required, those for which there is a need for a change in blade or use of intubation stylet, and those for which there is a need for an alternative intubation technique.1 Physicians should prepare for and anticipate the difficult airway to avoid the “cannot intubate, cannot ventilate” situation, and a backup plan should be made for every intubation. Important aspects of the case to consider are whether the patient will be easily ventilated with bag-mask ventilation to maintain oxygenation, whether intubation is likely to be successful, and what backup plan is most appropriate for the patient.2
Various history and physical examination findings may help the physician identify and anticipate a difficult airway. Features that suggest that bag mask ventilation may be difficult are facial anomalies caused by trauma or congenital abnormalities, limited neck mobility, obesity, obstructive lung disease, upper airway swelling, and tracheal narrowing. External characteristics of the patient that suggest that the proceduralist may have a difficult time with obtaining a laryngoscopic view or intubating include limited mouth opening, short and inflexible neck, large tongue, palate abnormality, and abnormally long or short thyromental distance. Copious amounts of oral blood or secretions may block the laryngoscopic view.1,2
Partial airway obstruction, which is a common cause of difficult bag-mask ventilation, can present with multiple signs, depending on the anatomic location of the obstruction. Patient hoarseness or weak crying is suggestive of possible airway obstruction at the vocal cords. Inspiratory stridor is a high-pitched sound produced during inspiration in the setting of obstruction at the level of the upper trachea when extrathoracic obstruction worsens with negative intrathoracic pressures associated with inspiration.
This physical examination finding often is seen in croup or bacterial tracheitis, as well as laryngomalacia. Expiratory stridor is a high-pitched sound that is heard on expiration in the setting of obstruction of the lower trachea or bronchi when airways are compressed during forced expiration. Swelling of the lips or tongue is concerning for airway obstruction secondary to angioedema and anaphylaxis. “Red-flag” signs of severe to complete airway obstruction include sniffing or tripod position, drowsiness, altered mental status, markedly reduced or no air movement, severely increased work of breathing, and silent gagging or coughing. Complete airway obstruction rapidly progresses to unconsciousness and cardiorespiratory arrest.3
Congenital abnormalities may interfere with many aspects of rapid sequence intubation (RSI) leading to a difficult airway. Misshapen head or limited neck mobility interferes with positioning of the head to align the airway axis, making it difficult to perform bag-mask ventilation and obtain an optimal laryngoscopic view. Facial asymmetry or underdevelopment may lead to difficulty obtaining a seal with a bag-valve mask to perform ventilation.
A small oral aperture and/or cavity may make opening the mouth and laryngoscopy difficult. A large tongue may make bag-mask ventilation difficult by creating an airway obstruction and may complicate obtaining an optimal view during laryngoscopy. Laryngeal and subglottic abnormalities may complicate bag-mask ventilation or endotracheal intubation.4
Various scoring tools have been created to help the proceduralist prepare for intubation, although these tools have limited use in the setting of an emergent intubation of a critically ill patient with limited cooperation. One such tool is the Colorado Pediatric Airway Score, which is a detailed scoring system that takes multiple physical characteristics into account and, thus, is particularly useful in cases of congenital abnormalities.4
Many providers use the mnemonic “LEMON” for difficult airway assessment and rapid identification of patients who potentially may have a difficult airway. This tool was developed by emergency airway management researchers for use in adults with good predictive value, but evidence regarding effectiveness for the mnemonic’s use in the pediatric is lacking.5 The mnemonic is as follows:
- Look externally: The clinician should evaluate for external indications of a difficult airway. In the pediatric population, external signs of a difficult airway include congenital head or facial anomalies, facial trauma, neck masses or hematoma, small mouth, short neck, and obesity.
- Evaluate 3-3-2: The clinician should assess the patient’s mouth opening, thyromental distance, and thyrohyoid distance, all of which are anatomic distances that may predict difficult airway anatomy for intubation. Adequate mouth opening is the width of three of the patient’s fingers measured from maxillary canine to mandibular canine. Adequate thyromental distance is the width of three of the patient’s fingers, measured from the chin to the superior notch of the thyroid cartilage. Adequate thyrohyoid distance should be the width of two fingers measured from the mandible to the superior notch of the thyroid cartilage. If the distance is longer or shorter than these assigned metrics, the laryngoscopist may have difficulty visualizing the larynx.
- Mallampati score: The clinician should assess a Mallampati score. The Mallampati classification is a simple scoring system that uses the size of the mouth opening relative to the size of the tongue to provide an estimate of intraoral space and visibility during laryngoscopy and predict a difficult airway. A Mallampati score can be assessed by asking the patient to open the mouth and stick out the tongue if cooperative. A tongue blade may be used to assess the Mallampati score of an obtunded supine patient. Class I is defined as visible soft palate, uvula, and pillars. Class II is defined as visible soft palate and uvula. Class III is defined as visible soft palate and base of uvula. Class IV is when only the hard palate is visible. A Mallampati score of Class III or IV is predictive of a difficult airway.6 (See Figure 1.)
- Obstructed airway: Any indication of an obstructed airway, such as epiglottitis, anaphylaxis, foreign body obstruction, burns with airway involvement, or caustic ingestions, is predictive of a difficult airway because these disease processes can limit laryngoscopic view, hinder passage of the endotracheal tube, and limit adequate bag-mask ventilation.
- Neck mobility: Limited neck mobility, particularly neck extension, due to suspected cervical spine injury or congenital anomalies indicates a potentially difficult airway because of constraints on ability to achieve the sniffing position for optimal laryngoscopic view
Figure 1. Mallampati Scoring System |
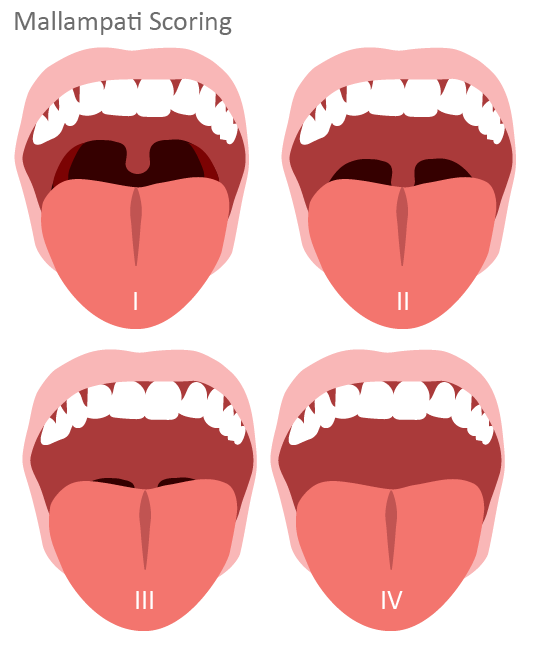 |
Source: Relias |
Another grading system that may help to predict difficulty passing the endotracheal tube through the vocal cords into the trachea is the modified Cormack-Lehane classification system. This classification system describes the best possible laryngeal view during laryngoscopy with optimal head and neck positioning, optimal blade length and position, optimal paralysis or muscular relaxation with minimization of glottic reflexes, and optimal laryngeal manipulation, if used. A Cormack-Lehane grade I view describes a laryngoscopic view in which the glottis is able to be fully visualized. The modified Cormack-Lehane further divides the grade II view. A grade IIa view describes a partial view of the vocal cords, whereas a grade IIb view describes a view in which only the arytenoids or the posterior origin of the cords is visible. A grade III view describes a laryngoscopic view in which only the epiglottis is visible. A grade IV describes a view in which no portion of the laryngeal structure is invisible. Laryngoscopy and passage of the endotracheal tube into the trachea is much more difficult when the laryngoscopist is unable to visualize the cords. Using this grading system, grade IIb through IV views are described as difficult laryngoscopies and are classified as difficult intubations.7
Pediatric Airway Obstruction
Difficult airways in children caused by partial airway obstruction should be managed very carefully. Small changes to the already smaller airway diameter of children significantly increase airway resistance. In a crying, agitated child, airflow also becomes turbulent, exponentially increasing airway resistance. In these scenarios, it is best to keep the child calm in a quiet, comfortable environment with minimal stimulation until they are able to be taken to the operating room. There, the airway should be managed in a controlled setting by consultants, such as anesthesiology or otolaryngology.8
Upper Airway Infections
Upper airway infections that cause upper airway edema and obstruction are common causes of difficult airway in children.
- Epiglottitis causes rapidly progressive inflammation and edema of supraglottic structures, leading to an extremely difficult airway scenario caused by narrowing of the glottic opening. Because of the distortion of the airway anatomy, supraglottic airways generally should be avoided. These children should be kept calm and upright until they are able to be taken to an operating room for airway management, although in a crash setting, a cricothyrotomy may be necessary.9
- Croup leads to subglottic airway obstruction and edema, which results in difficulty with bag-mask ventilation, placement of a supraglottic airway, and passage of an endotracheal tube through the subglottic trachea. Croup typically responds to medical management, including racemic epinephrine and dexamethasone, and rarely requires advanced airway management. Bacterial tracheitis leads to similar subglottic swelling, although the patient appears more toxic and typically does not respond to racemic epinephrine. If the patient requires intubation, the proceduralist should use an endotracheal tube that is one-half size smaller than normal for the patient’s age or size to account for airway narrowing caused by swelling and inflammation.10
- Ludwig angina is a life-threatening form of bacterial cellulitis of the submandibular tissues that is most often caused by dental infections of the mandibular molars. It can progress rapidly and result in airway obstruction and asphyxiation. Early recognition and intervention to secure a definitive airway is crucial given the rapidly progressive nature of the infection. Because of the submandibular swelling, both bag-mask ventilation and direct or video laryngoscopy are difficult, and supraglottic airways should be avoided. The preferred method of intubation is with a fiberoptic scope, although in a crash setting, a cricothyrotomy may be necessary.11
Anaphylaxis
Anaphylactic reactions can cause mucosal swelling of the airway involving the tongue, retropharynx, and larynx, which makes obtaining a laryngoscopic view of the vocal cords and bag-mask ventilation difficult. Medical management with corticosteroids, epinephrine, and histamine blockers helps to reduce swelling and symptoms. However, severe anaphylactic reactions may require intubation, and early airway management is crucial because any delay may reduce the chances of a successful intubation as continued swelling occurs. Signs of airway involvement that should prompt the clinician to obtain a definitive airway include perioral edema, stridor, and angioedema. Because laryngoscopy often is difficult in these patients because of mucosal swelling, the physician should consider fiberoptic intubation. The clinician should be equipped with a backup plan in the setting of failed intubation attempts; needle cricothyrotomy or surgical cricothyrotomy may be necessary if the patient cannot be ventilated or intubated.12
Hereditary Angioedema
Hereditary angioedema is a genetic disorder that causes soft tissue swelling secondary to decreased levels or function of complement C1 esterase inhibitor. The clinical presentation of hereditary angioedema consists of recurrent episodes of soft tissue swelling in the eyes, lips, and tongue. Treatment involves administration of C1 esterase inhibitor. Antihistamines, epinephrine, and corticosteroids are not effective in reducing swelling secondary to hereditary angioedema. Hereditary angioedema occasionally can present with airway edema, causing airway obstruction. Because the airway edema can progress rapidly, any signs of airway compromise should prompt the clinician to obtain a definitive airway. Laryngoscopy often is difficult in these patients because of mucosal swelling, so the physician should consider fiberoptic intubation and be prepared for possible surgical cricothyrotomy, as well as involve airway consultants, including anesthesia or otolaryngology, if available. Prompt administration of C1 esterase inhibitor concentrate is the most effective means of stopping progression of laryngeal edema in patients with hereditary angioedema, but that should not delay securing a definitive airway.13
Laryngospasm
Laryngospasm is a sudden involuntary closure of the vocal cords that is caused by a protective reflex, leading to airway obstruction and potentially resulting in significant hypoxia and bradycardia. In the emergency department setting, laryngospasm often is seen in patients who are undergoing conscious sedation for a procedure. However, any direct stimulation of the larynx may trigger this reflex, including airway secretions, intubation, and extubation. Clinical signs of laryngospasm include inspiratory stridor, which may progress to complete obstruction and desaturation. Laryngospasm should be suspected whenever sudden airway obstruction occurs in the absence of an obvious supraglottic cause.14,15
The first step of management of laryngospasm is removal of any triggering stimulation followed by performance of a vigorous jaw thrust maneuver to lift the tongue off the pharyngeal wall and lift the supraglottic tissues from the false vocal cords. The patient should then receive continuous positive airway pressure with 100% oxygen. Any secretions within the airway should be cleared using suction. Anecdotal evidence suggests that painful inward pressure at the Larson’s point or laryngospasm notch to the bilateral styloid processes behind the rami of the mandible performed spontaneously with the jaw thrust maneuver may help to stop the laryngospasm.15 Pharmacologic management should first be attempted with deepening of sedation with propofol using a dose of 0.25 mg/kg to 0.8 mg/kg. If the laryngospasm does not rapidly improve with sedation, then paralysis with succinylcholine at a dose of 0.1 mg/kg to 3 mg/kg together with atropine at 0.02 mg/kg to avoid succinylcholine-induced bradycardia should occur. Smaller doses of succinylcholine maintain spontaneous breathing but often stop the laryngospasm. If these methods are unsuccessful in improving the patient’s respiratory status, then the clinician should prepare to intubate using RSI.14,15
Laryngomalacia
Laryngomalacia is a congenital laryngeal disorder in infants defined as a collapse of supraglottic structures during inspiration, leading to upper airway obstruction and causing inspiratory stridor that worsens while supine and, in severe cases, episodes of apnea. This condition typically resolves without intervention between the ages of 18 to 24 months, but severe cases may require surgical intervention.16
Patients with known laryngomalacia are considered to have difficult airways because their pathophysiology results in challenges with both bag-mask ventilation and endotracheal intubation. Induction with a paralytic and loss of muscle tone may lead to airway collapse, which hinders bag-mask ventilation. Floppy epiglottic tissues often obscure the view of the vocal cords during laryngoscopy, leading to difficulty with visualizing the vocal cords and passing the endotracheal tube. In patients with laryngomalacia, intubation should be attempted using mild sedation and delayed paralysis if clinicians are able to preserve the respiratory drive. Reasonable considerations for the first attempt may be video laryngoscopy or fiberoptic scope intubation. If unsuccessful, the clinician may attempt to move the floppy epiglottis aside from the view of the glottis using a rigid bronchoscope if available and pass a bougie into the trachea with passage of the endotracheal tube over the bougie. An alternative method that may be attempted is endotracheal intubation using video laryngoscopy with the patient in a lateral position, which helps to prevent the airway collapse and moves the epiglottis away from the view of the vocal cords. If these attempts fail and the clinician is unable to intubate or ventilate the patient, a needle cricothyrotomy may be necessary.17,18
Foreign Body Obstruction
A common presentation to the pediatric emergency department is inhaled or aspirated foreign body. In the majority of cases, children spontaneously clear the obstruction with coughing. Aspirated foreign bodies most often become lodged within the bronchi and are not immediately life-threatening. Rarely, the foreign body may become trapped with the larynx or trachea and cause complete or partial airway obstruction that requires immediate airway management.
Foreign body obstructions that create a partial airway obstruction should be managed with expectant management until the patient is able to be taken to the operating room for endoscopic removal. Complete obstruction by a foreign body in a conscious patient should be managed with abdominal thrusts for children 1 year of age or older or five back blows followed by five chest thrusts with interspersed attempts at ventilation in infants. If the child becomes unresponsive, the clinician should start with 30 chest compressions and then reevaluate the airway. If the foreign body is visible, attempt to remove it from the oral cavity; avoid blind finger sweeps because they may push the foreign body downward toward the larynx.19
Direct laryngoscopy may be performed with an attempt to remove the foreign body with Magill forceps if it is supraglottic. If the foreign body is visualized above the vocal cords and causing compete obstruction of the airway but unable to be removed, an emergency surgical airway should be obtained. If unable to visualize the foreign body, the clinician may attempt intubation with an endotracheal tube to push the foreign body into the mainstem bronchus with subsequent withdrawal of the endotracheal tube above the carina to allow for temporary ventilation of the other lung until removal via bronchoscopy is able to occur.19
Trauma and Mucosal Injury
Both blunt and penetrating trauma may lead to upper airway obstruction in the setting of traumatic injury to the face and neck, leading to soft tissue swelling or hemorrhage and airway compromise — as well as because of direct blunt or penetrating trauma to the larynx or trachea. Expanding neck hematomas may continue to expand and create an airway obstruction. Airway trauma can deteriorate quickly, so the physician should prepare for intubation with video laryngoscopy, fiberoptic intubation, or, if necessary, emergency surgical cricothyrotomy, and intervene early at the first sign of respiratory compromise. Emergency consultation with otolaryngology or anesthesiology should occur, if available.20
Thermal injury and chemical injury to the airway can lead to a significant amount of rapidly developing edema and, eventually, complete airway obstruction. Physicians should be on high alert for thermal injury to the airway when there are significant facial burns or singed nasal hairs. In patients who present after a caustic ingestion, physicians should evaluate for any signs of airway involvement, including drooling and difficulty tolerating secretions, hoarse or dysphonic voice, and increased work of breathing. Evaluation for airway edema can be performed using fiberoptic bronchoscopy. With airway edema caused by burns or caustic injuries, intubation should occur at the first sign of respiratory involvement or with airway edema noted on bronchoscopy. Physicians may need to intubate via fiberoptic intubation and should prepare for possible surgical cricothyrotomy as well as consult otolaryngology or anesthesiology, if available.21
Difficult Bag-Mask Ventilation Techniques
The ability to perform effective bag-mask ventilation is extremely important for successful airway management, especially in children with lower oxygen reservoirs and higher potential to desaturate during intubation. Difficulty with bag-mask ventilation increases the risk for severe adverse events associated with intubation, including hypoxia and death. If the provider anticipates difficulty with bag-mask ventilation, then an awake fiberoptic approach to intubation without paralysis should be considered. If difficulty with bag-mask ventilation is encountered, the provider should attempt to optimize positioning and technique.
Optimize Positioning and Equipment
The optimal positioning for ventilation in children is the sniffing position, which improves airway patency by aligning the oral, pharyngeal, and laryngeal axes. Externally, the sniffing position ideally is achieved when the ear and sternal notch are aligned in the same plane. Airway maneuvers to achieve optimal positioning include the head tilt-chin lift and the jaw thrust maneuvers.22
The head tilt-chin lift maneuver is the initial approach to minimizing anatomic obstruction by the tongue and opening the airway for adequate ventilation. Place a hand on the child’s forehead and gently tilt the head backward. Then, place the fingers under the chin and lift gently upward to move the mandible anteriorly. Caution should be taken to avoid hyperextending the neck or applying pressure to the soft tissues underneath the mandible, both of which may worsen obstruction.22,23 The jaw thrust maneuver should be used in trauma patients with a suspected cervical spine injury. To perform, hook the thumbs behind the angles of the mandible and move the mandible forward. If still unable to achieve adequate ventilation with this position, then gently attempt head tilt-chin lift maneuver while maintaining in-line cervical spine stabilization.22,23
Placing a rolled towel underneath the shoulders in infants or underneath the occiput in children older than 2 years of age may help to maintain the ideal sniffing position.24
Additionally, the provider should check the sizing of the mask. A properly sized mask is crucial to ensure adequate ventilation. The mask should cover the nose but not the eyes, and the lower border of the mask should rest on the chin to provide an airtight seal that covers the entirety of the nose and the mouth.22
Finally, the clinician should evaluate the airway for any obstruction by secretions or airway debris and attempt to suction the oropharyngeal airway to clear debris and improve ventilation. Prolonged suctioning should be avoided, since it may lead to hypoxia and bradycardia.25
Two-Person Ventilation
Two-person bag-mask ventilation is a ventilation technique that requires two rescuers. One person uses the “E-C” technique with both hands while another person squeezes the bag. The two-person technique has been shown to provide a better seal on the mask and provide a higher tidal volume to the patient with each squeeze.26
To perform two-rescuer ventilation, one rescuer holds the mask to the face using the “E-C” configuration with the thumb and second finger of each hand forming a “C” shape onto the mask to press the mask into the child’s face and form a seal between the mask and face and the third through fifth fingers spread along the mandible, with the fifth finger behind the angle of the mandible working to lift the jaw and pull the face into the ventilation mask. The focus should be pulling the airway up into the mask rather than pushing the mask down into the face. Care should be taken to apply pressure to the bony aspect of the mandible rather than the submandibular tissue because pressing on these soft tissues can lead to airway obstruction by the tongue.22
Airway Adjuncts
If the provider continues to face difficulty with ventilation despite troubleshooting position, equipment, and technique, various airway adjuncts exist to help relieve anatomical obstruction and assist with bag-mask ventilation.
If the child is sedated or unconscious and has no gag reflex, an oropharyngeal airway may be used to push the tongue away from the posterior pharynx and open the airway. This airway adjunct is especially helpful in children with a large tongue or poor pharyngeal tone. Because oropharyngeal airways have the potential to trigger the gag reflex, they should not be used in awake patients, since they may increase the risk for vomiting and aspiration. The size of the oropharyngeal airway can be chosen by measuring the distance from the corner of the mouth to the angle of the mandible. These devices are placed by depressing the tongue with a tongue blade and gently inserting the oropharyngeal airway along the curve of the mouth and pharynx.27
If the child is awake and has an intact gag reflex or has limited mouth mobility, a nasopharyngeal airway should be used instead. This airway adjunct works by removing anatomic obstruction by displacing the tongue from the posterior pharynx. To approximate the correct size of a nasopharyngeal airway, the distance from the tip of the nose to the ear tragus should be measured. These devices are placed by lubricating the nasopharyngeal tube and gently inserting into the larger nostril in a posterior direction with the bevel facing the nasal septum.28
Gastric Insufflation
A common pitfall of bag mask ventilation is insufflation of the stomach. In turn, the stomach inflates with air and presses against the diaphragm, limiting the tidal volume able to be delivered. To prevent gastric distention, low pressure low volume breaths should be delivered.22
Difficult Pediatric Airway Techniques
Many techniques exist for the management of a difficult pediatric airway. The proceduralist always should be prepared with a backup airway plan for an anticipated difficult airway, with appropriate corresponding equipment readily available when the decision is made to intubate. The decision on backup plan and techniques in the setting of a failed endotracheal intubation should be based on the clinical scenario.
Supraglottic Airway
Supraglottic airway devices should be used when intubation attempts fail and bag-mask ventilation is inadequate.29 These devices create a seal superior to the glottic opening to allow for adequate oxygenation and ventilation. However, they do not provide as much protection against aspiration as a definitive airway. Laryngeal mask airways (LMAs) should be avoided in patients with airway obstruction, such as in croup or asthma, and in patients with distorted airway anatomy because of trauma or congenital conditions.30
Multiple forms of supraglottic airways are available and appropriate for use in children. The LMA sits over the glottic opening and has an inflatable cuff to provide a seal. The i-gel is shaped similarly to the LMA but has a soft plastic cuff instead of an inflatable cuff. The King laryngeal tube is another supraglottic airway device with two balloons to provide a seal in the esophagus and the oropharynx with a tube opening that points toward the glottis.31
To place a supraglottic airway, select the appropriately sized device. Apply a water-soluble lubricant to the supraglottic airway. Open the patient’s mouth using a similar scissor technique as used in intubation. Insert the device by gently gliding it along the hard palate until resistance is met. Inflate the cuff or balloon, if applicable. Then, initiate bag-mask ventilation and use end-tidal carbon dioxide to confirm correct supraglottic device placement. Secure the device using tape. In some cases during insertion of the supraglottic device, the epiglottis will fold over the glottic opening, resulting in an air leak through the mouth. In this case, remove the device, optimize the position of the patient, and reattempt insertion.30
Video Laryngoscopy
Video laryngoscopy has become used more frequently for the first attempt of pediatric intubations, and if the first attempt is performed using direct laryngoscopy, it is reasonable to switch to video laryngoscopy. It Is important for the provider to note that video laryngoscopy blades are bulkier than those for direct laryngoscopy. Therefore, maneuvering the endotracheal tube into the correct position between the vocal cords despite an optimal laryngoscopic view may be more difficult.32
Gum Elastic Bougie
The gum elastic bougie is a device that is a semi-rigid rod with the distal tip bent at a 30-degree angle to allow the laryngoscopist to direct the tip anteriorly under the glottis and through the vocal cords and later verify tracheal placement through palpation of the tracheal rings.33 This introducer is useful to assist with endotracheal intubation when the laryngoscopist is able to visualize the epiglottis but unable to obtain a full view of the vocal cords. This technique is most useful in facilitating intubation of patients with Cormack-Lehane grade III glottic view; in such scenarios, when the laryngoscopist is unable to obtain a full visualization of the glottis, the gum elastic bougie introducer may increase the first-pass success rate. The bougie introducer is contraindicated in patients with laryngeal or tracheal injury.34,35
To use the gum elastic bougie, the clinician should first obtain the best possible laryngoscopic view of the arytenoid cartilages, then insert the angled tip of the gum elastic bougie through the glottis with the angled tip directed anteriorly. If the bougie is in the trachea, then the laryngoscopist will feel the tip of the bougie vibrating as it passes along the tracheal rings. Once the bougie is in the trachea, the endotracheal tube can be threaded over the bougie. Difficulty passing the endotracheal tube may be encountered by the epiglottis blocking further advancement. This problem may be overcome by rotating the endotracheal tube 90 degrees as it approaches the larynx. Once the endotracheal tube is in the trachea, the cuff should be inflated if applicable, and then the gum elastic bougie should be removed. Placement of the endotracheal tube should be confirmed using an end-tidal carbon dioxide detector secured and attached to the bag-mask ventilation or ventilator.36
Fiberoptic Scope Intubation
Fiberoptic scopes are malleable stylets with a camera at the tip that may be used to transmit an image to the operator of the machine. These machines can be used to perform visually guided intubation in patients for whom direct or video laryngoscopy is anticipated to be difficult because of limited neck mobility or a difficult laryngoscopic view.35 The flexible intubating scope also may be used for patients with a difficult airway who are breathing spontaneously through a procedure called awake fiberoptic intubation. This method should be considered in patients who are anticipated to be difficult to ventilate and intubate during RSI and are able to tolerate a longer intubation attempt. In children, this method may be considered in patients with congenital airway anomalies or in cases with anticipated difficulty of alignment of the airway axes for positioning. The main pitfall of this method is that it limits the size of the endotracheal tube that can be used. Most standard endoscopes will fit endotracheal tubes that are more than 5.5 mm in diameter. Additionally, flexible endoscopic intubation requires a calm, cooperative patient, which limits its use in many clinical scenarios.2,37
To perform an awake fiberoptic intubation, the provider should first ensure the child is comfortable and cooperative or lightly sedated. Adequate topical airway anesthesia should be given, typically in the form of nebulized or viscous lidocaine.38 Additionally, the patient may be given light sedation using ketamine, dexmedetomidine, or propofol, depending on the clinical scenario with the intent to keep the patient calm but also maintain spontaneous respirations. Glycopyrrolate may be given in an intravenous form to reduce and minimize airway secretions.39 Fentanyl also may be given as a pretreatment to blunt the sympathetic response to intubation attempts and minimize pain.
Prior to attempting intubation, the patient should be preoxygenated with 100% oxygen via face mask. Next, the flexible scope should be inserted through the mouth or nose to visualize the vocal cords. Once the vocal cords are visualized, the scope should be advanced through the vocal cords and into the trachea. The endotracheal tube should be passed over the scope into the trachea. The clinician may use the scope to confirm placement of the endotracheal tube by visualizing the carina beyond the end of the tube. The scope should be withdrawn while holding the endotracheal tube steady, and then the endotracheal tube should be secured, confirmed with colorimetry, and connected to the ventilator.40,41
Surgical Airways
When laryngoscopic intubation and rescue airway attempts have failed and the patient cannot be ventilated and oxygenated, the final airway solution is cricothyrotomy. Cricothyrotomy is the process of inserting a catheter or endotracheal tube percutaneously into the trachea through the cricothyroid membrane via incision or needle to obtain access to the patient’s airway for ventilation and oxygenation. Timely recognition and intervention of a “cannot intubate, cannot ventilate” scenario is extremely important — failure to do so can rapidly lead to brain hypoxia and death.42
Cricothyroid Membrane Anatomy
To successfully perform a needle cricothyrotomy or open surgical cricothyrotomy, the clinician should understand the relevant anatomy to palpate the cricothyroid membrane. The cricothyroid membrane is anatomically located between the superior thyroid cartilage and the inferior cricoid cartilage, bordered laterally by the bilateral cricothyroideus muscles.
To locate the cricothyroid membrane, the laryngeal prominence or “Adam’s apple” on the thyroid cartilage should first be palpated. Next, the clinician should palpate the round signet ring located inferior to the laryngeal prominence. The cricothyroid membrane is located between these two landmarks and can be identified as a slight depression between the two cartilaginous structures.42
Needle Cricothyrotomy
Because of the small cricothyroid membrane and increased risk of laryngeal injury, open surgical cricothyrotomy is contraindicated in children younger than 10 years of age. Instead, children younger than 10 to 12 years of age should undergo needle cricothyrotomy in “cannot intubate, cannot ventilate” scenarios.
Needle cricothyrotomy involves passing a catheter over a needle through the cricothyroid membrane into the trachea through which temporary oxygenation and ventilation can be provided. This method is a temporizing measure until definitive airway management can be achieved. A needle cricothyrotomy will provide adequate oxygenation but does not provide adequate ventilation.43
To perform the procedure, the clinician should first clean the skin, then locate the cricothyroid membrane. Then, use the non-dominant thumb and middle finger to spread the skin overlying the cricothyroid membrane to palpate the cricothyroid membrane with the pointer finger and stabilize the larynx. Next, the provider should use a 3-mL syringe filled with saline attached to a 14-gauge angiocatheter to pierce through the cricothyroid membrane directed caudally at an angle of 30 to 45 degrees. Continuous negative pressure should be applied to the syringe while advancing until air bubbles are visualized within the syringe, confirming placement within the trachea. The clinician should stop advancing the needle and advance the catheter over the needle until the hub abuts the skin. Then, remove the needle, holding the catheter steady. The saline syringe then should be attached to the catheter, and tracheal placement should be confirmed by aspirating air into the syringe. Once placed in the trachea, the catheter should be held in place at all times to maintain correct positioning. The catheter should be connected to high-pressure tubing or a bag valve mask attached to 100% oxygen. Ventilation should be performed with a rate of 10 to 12 breaths per minute using an inspiratory to expiratory ratio of approximately 1:4.42,43 (See Figure 2.)
Figure 2. Needle Cricothyrotomy |

 |
Top: Insertion of the needle through the cricothyroid membrane Bottom: Ventilating through a needle cricothyrotomy with a bag-valve mask Courtesy of Dr. Alexandra Armato and Dr. Daniel Migliaccio. |
Jet ventilation frequently is taught as an alternative method to ventilation with a bag mask. Jet ventilation is achieved by attaching high-pressure oxygen tubing directly to wall-mounted oxygen. For children 0 to 5 years of age, use pressures of < 20 mmHg. For children 5 to 12 years of age, use pressures of < 30 mmHg. Finally, for patients 12 years of age and older, use pressures of < 50 mmHg. Use an inspiratory to expiratory ratio of 1:4 to 1:5, with a breath rate of 10 to 12 per minute. Jet ventilation rarely is used in practice, given high risk for barotrauma.42
When ventilating through a catheter in a patient after needle cricothyrotomy, known as percutaneous transtracheal ventilation, much of the expired air comes out through the oral and nasal cavity, given the small diameter of the needle relative to the airway. However, air is not able to travel upward through a complete airway obstruction during the expiratory phase, which can lead to development of massive distention of the lungs, severe barotrauma, and death. In patients with complete airway obstruction, modified techniques — including prolonged expiratory time, lower oxygen delivery pressure, and use of a catheter with a larger internal diameter — should be considered to reduce the risk of these complications. The chest wall should be monitored during percutaneous transtracheal ventilation for both chest rise during the inspiratory phase and chest fall during the expiratory phase.42,44
A definitive airway with an endotracheal tube or tracheostomy should be obtained as soon as possible after a needle cricothyrotomy is performed. Complications of prolonged percutaneous transtracheal ventilation include excessive inspiratory workload with distention of the lungs, hypoventilation with hypercapnia, barotrauma, subcutaneous emphysema, and catheter dislodgment. The traditionally accepted amount of time between initiation of percutaneous transtracheal ventilation and establishment of a definitive airway is no longer than 45 minutes. If available, anesthesia or otolaryngology should be involved, especially in patients with traumatic injuries to the face or neck. If those consultants are unavailable or, in certain non-traumatic cases, the emergency practitioner should attempt establishment of a definitive airway using a laryngoscopic approach.43
Difficult Airway Adjuncts
Surgical cricothyrotomy is the emergency airway technique of choice in patients older than 10 to 12 years of age. This procedure involves making an incision in the cricothyroid membrane and passing an endotracheal tube or a tracheostomy through the incision. Because of the larger diameter of the endotracheal tube placed within the trachea, open surgical cricothyrotomy provides more effective ventilation than needle cricothyrotomy.2,42
To perform surgical cricothyrotomy, the skin of the anterior neck should be cleaned with chlorhexidine or iodine, then the clinician should locate the cricothyroid membrane with the index finger and stabilize the larynx between the thumb and middle finger of the non-dominant hand. Next, an approximately 4-cm vertical incision should be made through the skin overlying the cricothyroid membrane.42
The clinician then should use the fingers to bluntly dissect through the subcutaneous tissue until the cricothyroid membrane is identified. Bleeding is common and to be expected at this point, and obtaining the airway should take priority. Next, a midline horizontal incision through the cricothyroid membrane should be created using a scalpel, and the clinician should insert the left index finger into the trachea and dilate. A gum elastic bougie then should be inserted into the trachea, and the clinician should use the index finger to guide it inferiorly. The clinician then should remove the finger, holding the gum elastic bougie steady with the other hand, and pass a size 6.0, cuffed endotracheal tube over the bougie until the balloon is no longer visible. Then, inflate the cuff. Placement of the endotracheal balloon should be confirmed using an end tidal carbon dioxide detector. The endotracheal tube should be secured in place using a securement device, and ventilation with a bag-valve mask or ventilator should be initiated. If severe bleeding occurs, the clinician should use pressure or packing at the site of the bleeding to provide hemostasis.42 (See Table 1.)
Table 1. Difficult Airway Tools/Techniques |
| Gum Elastic Bougie |
|
| Supraglottic Airways |
|
| Fiberoptic Scope Intubation |
|
| Surgical Airway |
|
Ultrasound Identification of Cricothyroid Membrane
Physical palpation of the neck to identify the cricothyroid membrane can be difficult, especially in children’s smaller anatomies. Precise cricothyroid membrane localization is vital, especially in the “cannot intubate, cannot ventilate” scenario. Bedside ultrasound has been shown to be superior in the identification of the cricothyroid membrane over a landmark technique. Providers may use an ultrasound to locate the cricothyroid membrane and mark the correct surgical site prior to performing cricothyrotomy. In cases with unconvincing landmark identification, such as in morbidly obese patients, ultrasound identification of the cricothyroid membrane is especially helpful. However, this technique takes longer than landmark palpation, so providers may find it difficult to apply this technique in a crash airway scenario. As the use and popularity of bedside ultrasound continues to grow in emergency medicine, the use of ultrasound in the setting of a difficult airway may continue to expand.45
Approach to the Difficult Pediatric Airway
When a difficult airway is anticipated, always consider consulting with otolaryngology or anesthesiology to perform or have on standby. The next important question is whether bag-mask ventilation will be difficult. If bag-mask ventilation is anticipated to be difficult and an awake approach is feasible in a calm and cooperative child who will tolerate a longer intubation attempt, proceed with fiberoptic awake intubation. If bag-mask ventilation is not anticipated to be difficult or the patient is anticipated to be difficult to ventilate but is not suitable for an awake intubation attempt, proceed with RSI.
Prior to initiating induction, gather supplies for airway adjuncts to assist with ventilation and intubation if needed; have a gum elastic bougie, oropharyngeal or nasopharyngeal airways, laryngeal mask airway, and supplies for needle or open cricothyrotomy readily available at bedside. After induction, place the patient’s head in the optimal position and perform jaw thrust and tilt-chin lift maneuvers as appropriate. Attempt intubation using video laryngoscopy, the gum elastic bougie technique, or fiberoptic intubation.
If the patient cannot be intubated, declare a failed intubation out loud to inform team members that there is an airway problem, then allow them to refocus and assist. Remove the laryngoscopic tool and ventilate to restore oxygen reserve if mask ventilation is possible. Consider placing a laryngeal mask airway to assist with ventilation and oxygenation or, if the patient is continuing to ventilate well, troubleshoot intubation with alternative options using a different laryngoscopy blade or different airway technique than the initial attempt. If mask ventilation becomes inadequate, attempt to troubleshoot by using a two-person two-hand technique for bag-mask ventilation, optimizing jaw thrust and chin lifts, placing an oropharyngeal or nasopharyngeal airway, or inserting an LMA or other supraglottic device. Consider laryngospasm and treat accordingly by deepening sedation if there is high suspicion for it. If anesthesiology or otolaryngology is not yet aware of the patient, call for help from consultants. Limit the number of intubation attempts to three because repeated intubation attempts can lead to tracheal injury, bleeding, and edema and may delay ventilation and establishment of a definitive surgical airway. If the patient cannot be ventilated or intubated, declare a “cannot intubate, cannot ventilate” scenario to alert team members and to allow them to refocus and assist.
Maximize oxygenation with apneic oxygenation or high-flow nasal cannula and prepare for a surgical airway or cricothyrotomy. Open surgical airways provide a definitive airway, but needle cricothyrotomies (as required for children younger than 10 years of age) are a temporizing measure, so once performed, work to obtain definitive airway in these patients.2 (See Figure 3.)
Figure 3. Difficult Airway Algorithm |
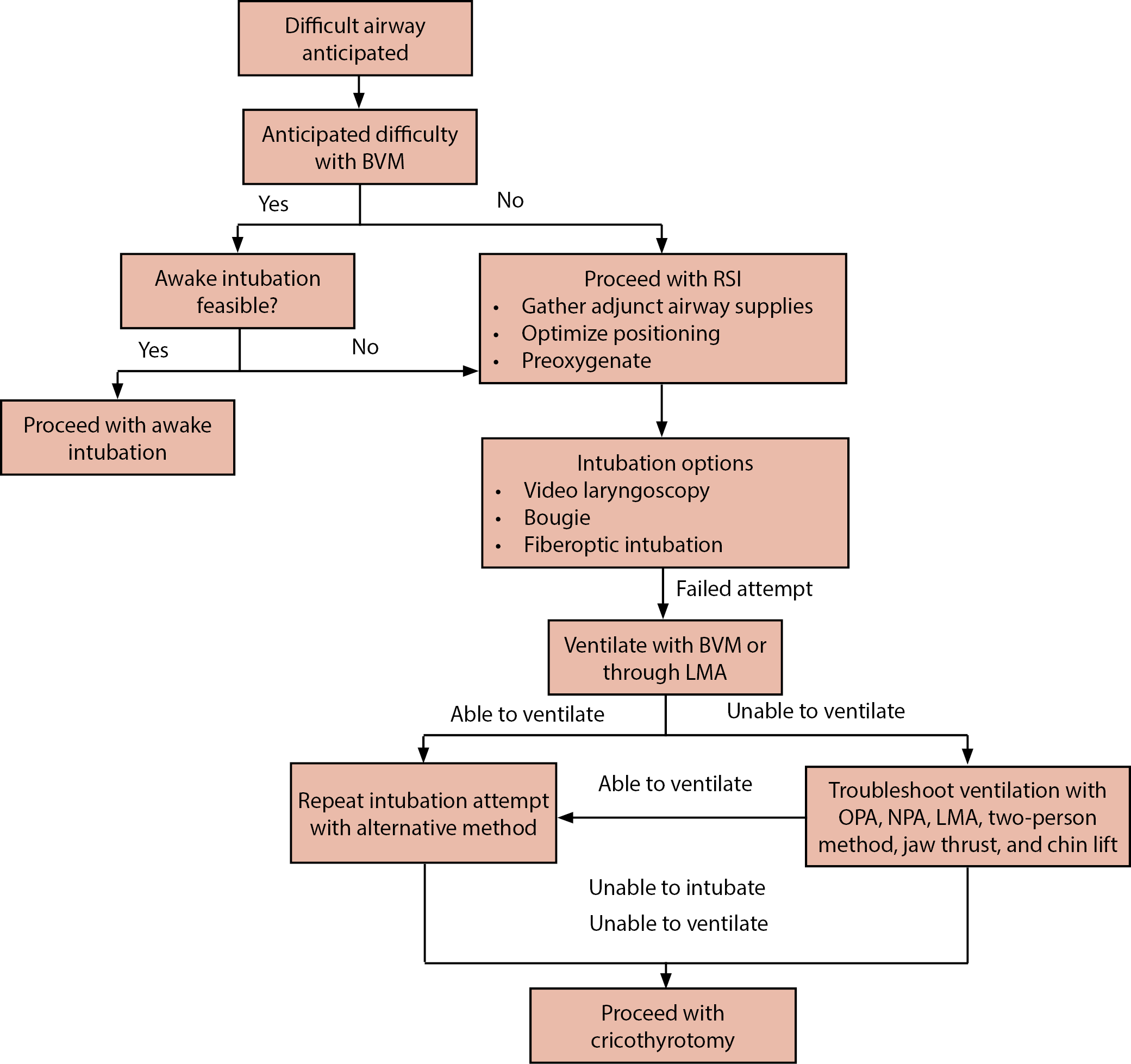 |
BVM: bag-valve mask; RSI: rapid sequence intubation; LMA: laryngeal mask airway; OPA: oropharyngeal airway; NPA: nasopharyngeal airway |
Conclusion
Managing a difficult airway requires a multifaceted approach that allows providers to use their knowledge and advanced airway techniques to overcome complications with pediatric airways. Having an understanding of difficult pediatric airway concepts will allow teams in pediatric emergency departments to ensure optimal patient outcomes despite a challenging situation.
Alexandra Armato, MD, is a resident at the Department of Emergency Medicine at University of North Carolina at Chapel Hill.
Daniel Migliaccio, MD, FPD, FAAEM, is a clinical associate professor, division director of emergency ultrasound, ultrasound fellowship director, Department of Emergency Medicine, University of North Carolina at Chapel Hill.
References
- Huang AS, Hajduk J, Rim C, et al. Focused review on management of the difficult paediatric airway. Indian J Anaesth. 2019;63(6):428-436.
- Krishna SG, Bryant JF, Tobias JD. Management of the difficult airway in the pediatric patient. J Pediatr Intensive Care. 2018;7(3):115-125.
- EO Cathain, Gaffey MM. Upper airway obstruction. In: StatPearls [Internet]. Updated Oct 17, 2022. https://www.ncbi.nlm.nih.gov/books/NBK564399/
- Raj D, Luginbuehl I. Managing the difficult airway in the syndromic child. Continuing Education in Anaesthesia, Critical Care, and Pain. 2015;15:7-13.
- Hendrix JM, Patel R, Friede R. 3-3-2 rule. In: StatPearls [Internet]. Updated Aug. 17, 2023. https://www.ncbi.nlm.nih.gov/books/NBK493235/
- Stutz EW, Rondeau B. Mallampati score. In: StatPearls [Internet]. Updated Aug. 5, 2023. https://www.ncbi.nlm.nih.gov/books/NBK585119/
- Yentis SM, Lee DJH. Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anesthesia. 2002;53(11):1041-1044.
- Vijayasekaran S. Pediatric airway pathology. Front Pediatr. 2020;8:246.
- Sutton AE, Guerra AM, Waseem M. Epiglottitis. In: StatPearls [Internet]. Updated Oct. 5, 2024. https://www.ncbi.nlm.nih.gov/books/NBK430960/
- Kadam SJ, Daley SF, Carr B. Croup. In: StatPearls [Internet]. Updated July 24, 2023. https://www.ncbi.nlm.nih.gov/books/NBK431070/
- An J, Ghabra YAL, Singhal M. Ludwig angina. In: StatPearls [Internet]. Updated May 24, 2023. https://www.ncbi.nlm.nih.gov/books/NBK482354/
- McLendon K, Sternard BT. Anaphylaxis. In: StatPearls [Internet]. Updated Jan 26, 2023. https://www.ncbi.nlm.nih.gov/books/NBK482124/
- Farkas H. Management of upper airway edema caused by hereditary angioedema. Allergy Asthma Clin Immunol. 2010;6(1):19.
- Al-alami AA, Zestos MM, Baraka AS. Pediatric laryngospasm: Prevention and treatment. Curr Opin Anaesthesiol. 2009;22(3):388-395.
- Gavel G, Walker RWM. Laryngospasm in anaesthesia. Continuing Education in Anaesthesia Critical Care & Pain. 2013;14(2):47-51.
- Klinginsmith M, Winters R, Goldman J. Laryngomalacia. In: StatPearls [Internet]. Updated Jan. 10, 2024. https://www.ncbi.nlm.nih.gov/books/NBK544266/
- Sharma R, Dwivedi D, Choudhary R. Anesthesia challenges for emergency surgery in a pediatric patient with congenital laryngomalacia. Audi J Anaesth. 2018;12(3):500-502.
- Sannaboraiah SK, Ture P, Gangadharan AK, Hatyal RC. Airway challenges in an infant undergoing laser supraglottoplasty for laryngomalacia. Indian J Anaesth. 2023;67(2):230-231.
- Dodson H, Sharma S, Cook J. Foreign body airway obstruction. In: StatPearls [Internet]. Updated July 17, 2024. https://www.ncbi.nlm.nih.gov/books/NBK553186/
- Mercer SJ, Jones CP, Bridge M, et al. Systematic review of the anaesthetic management of non-iatrogenic acute adult airway trauma. Br J Anaesth. 2016;117(Suppl 1):i49-i59.
- Sabri A, Dabbous H, Dowli A, Barazi R. The airway in inhalational injury: Diagnosis and management. Ann Burns Fire Disasters. 2017;30(1):24-29.
- Bucher JT, Vashisht R, Cooper JS. Bag-valve-mask ventilation. In: StatPearls [Internet]. Updated May 21, 2023. https://www.ncbi.nlm.nih.gov/books/NBK441924/
- Chua C, Schmölzer GM, Davis PG. Airway manoeuvres to achieve upper airway patency during mask ventilation in newborn infants — An historical perspective. Resuscitation. 2012;83(4):411-416.
- Alfahel W, Gopinath A, Arheart KL, et al. The effects of a shoulder roll during laryngoscopy in infants: A randomized, single-blinded, crossover study. Anesth Analg. 2020;131(4):1210-1216.
- Tume LN, Copnell B. Endotracheal suctioning of the critically ill child. J Pediatr Intensive Care. 2015;4(2):56-63.
- Davidovic L, LaCovey D, Pitetti RD. Comparison of 1- versus 2-person bag-valve-mask techniques for manikin ventilation of infants and children. Ann Emerg Med. 2005;46(1): 37-42.
- Castro D, Freeman LA. Oropharyngeal airway. In: StatPearls [Internet]. Treasure Island Updated July 31, 2023. https://www.ncbi.nlm.nih.gov/books/NBK470198/
- Atanelov Z, Aina T, Smith T, Rebstock SE. Nasopharyngeal airway. In: StatPearls [Internet]. Updated Jan. 30, 2024. https://www.ncbi.nlm.nih.gov/books/NBK513220/
- Garcia-Marcinkiewicz AG, Lee KL, Haydar B, et al. Difficult or impossible facemask ventilation in children with difficult tracheal intubation: A retrospective analysis of the PeDI registry. Br J Anesth. 2023;131(1):178-187.
- Simon LV, Torp KD. Laryngeal mask airway. In: StatPearls [Internet]. Updated July 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK482184/
- Ramesh S, Jayanthi R. Supraglottic airway devices in children. Indian J Anaesth. 2011;55(5):476-482.
- Couto TB, Reis AG, Farhat SCL, et al. Changing the view: Video versus direct laryngoscopy for intubation in the pediatric emergency department. Medicine (Baltimore). 2020;99(38):e22289.
- Komasawa N, Hyoda A, Matsunami S, et al. Utility of a gum-elastic bougie for difficult airway management in infants: A simulation-based crossover analysis. Biomed Res Int. 2015;2015:617805.
- von Hellmann R, Fuhr N, Maia IWA, et al. Effect of bougie use on first-attempt success in tracheal intubations: A systematic review and meta-analysis. Ann Emerg Med. 2024;83(2):132-144.
- Kovacs G, Law JA, McCrossin C, et al. A comparison of a fiberoptic stylet and a bougie as adjuncts to direct laryngoscopy in a manikin-simulated difficult airway. Ann Emerg Med. 2007;50(6):676-685
- Alvarado AC, Panakos P. Endotracheal tube intubation techniques. In: StatPearls [Internet]. Updated July 10, 2023. https://www.ncbi.nlm.nih.gov/books/NBK560730/
- Wong J, Lee JSE, Wong TGL, et al. Fibreoptic intubation in airway management: A review article. Singapore Med J. 2019;60(3):110-118.
- Pirlich N, Lohse JA, Noppens RR. Topical airway anesthesia for awake-endoscopic intubation using the spray-as-you-go technique with high oxygen flow. J Vis Exp. 2017;(119):55116.
- Cho E-A, Hwang S-H, Lee S-H, et al. Does glycopyrrolate premedication facilitate tracheal intubation with a rigid video-stylet? A randomized controlled trial. Medicine (Baltimore). 2018;97(32):e11834.
- Kollmeier BR, Boyette LC, Beecham GB, et al. Difficult airway. In: StatPearls [Internet]. Updated April 10, 2023. https://www.ncbi.nlm.nih.gov/books/NBK470224/
- Hassan MH. Awake fiberoptic intubation in a pediatric patient with cervical spine injuries on a halo-vest: A case report. Anesthesia, Pain & Intensive Care. 2022;26(4):569-573.
- McMahon K, Tariq A, Morley EJ. Cricothyrotomy. In: StatPearls [Internet]. Updated Feb. 4, 2023. https://www.ncbi.nlm.nih.gov/books/NBK537350/
- Mace SE, Khan N. Needle cricothyrotomy. Emerg Med Clin N Am. 2008;26(4):1085-1101.
- Berry M, Tzeng Y, Marsland C. Percutaneous transtracheal ventilation in an obstructed airway model in post-apnoeic sheep. Br J Anesth. 2014;113(6):1039-1045.
- Alerhand S. Ultrasound for identifying the cricothyroid membrane prior to the anticipated difficult airway. Am J Emerg Med. 2018;36(11):2078-2084.