
Oral Health for the PCP: A Collaborative Approach to Patient Care
October 1, 2025
By Terry Schmunk, DDS, MPH
Executive Summary
This issue emphasizes the crucial role of primary care physicians in identifying, managing, and referring patients with oral health conditions. Since many systemic diseases first manifest in the oral cavity, early detection during routine physical exams can improve outcomes. It details common oral conditions, their clinical features, management approaches, and systemic implications, while reinforcing the importance of collaboration between medical and dental professionals.
- Conditions such as diabetes, cardiovascular disease, and autoimmune disorders may present with early signs in the mouth.
- Recognizing features of leukoplakia, lichen planus, thrush, geographic tongue, syphilitic chancres, and angular cheilitis is essential for timely referral.
- Persistent oral leukoplakia warrants urgent evaluation because of its precancerous potential.
- Chronic gum disease is strongly associated with cardiovascular disease, highlighting the need for proactive management.
- Counseling patients on oral hygiene, nutrition, and lifestyle (e.g., smoking and alcohol cessation) significantly reduces oral and systemic disease burden.
Oral examinations are an essential component of a comprehensive physical examination and should be integrated into routine primary care practice for each patient. A comprehensive oral examination by a physician is paramount for good health. Only 45% of Americans see a dentist each year, and these individuals usually are those with dental insurance or who are more financially stable.1
Primary care physicians play a key role in the early detection of systemic disease by assessing the oral health of their patients. The oral cavity may present early signs of conditions such as metabolic disorders, endocrine disorders, autoimmune diseases, and various malignancies. Neoplastic processes may manifest as metastatic lesions within oral soft tissues or bone. Chronic illnesses, including gastroesophageal reflux and eating disorders, also can result in distinct oral changes.
Given these associations, physicians must recognize oral manifestations as potential indicators of systemic disease. Timely recognition and referral to dental professionals can provide earlier diagnosis, targeted intervention, and improved outcomes.
Oral Health and Systemic Disease
Oral health is defined as the optimal state of the mouth, teeth, and orofacial structures, enabling essential functions such as eating, breathing, and speaking. (A numbered diagram of the teeth is shown in Figure 1.) It also encompasses psychosocial aspects, including self-confidence, well-being, and the ability to socialize and work without pain or discomfort.2,3
Figure 1. Diagram of the Teeth |
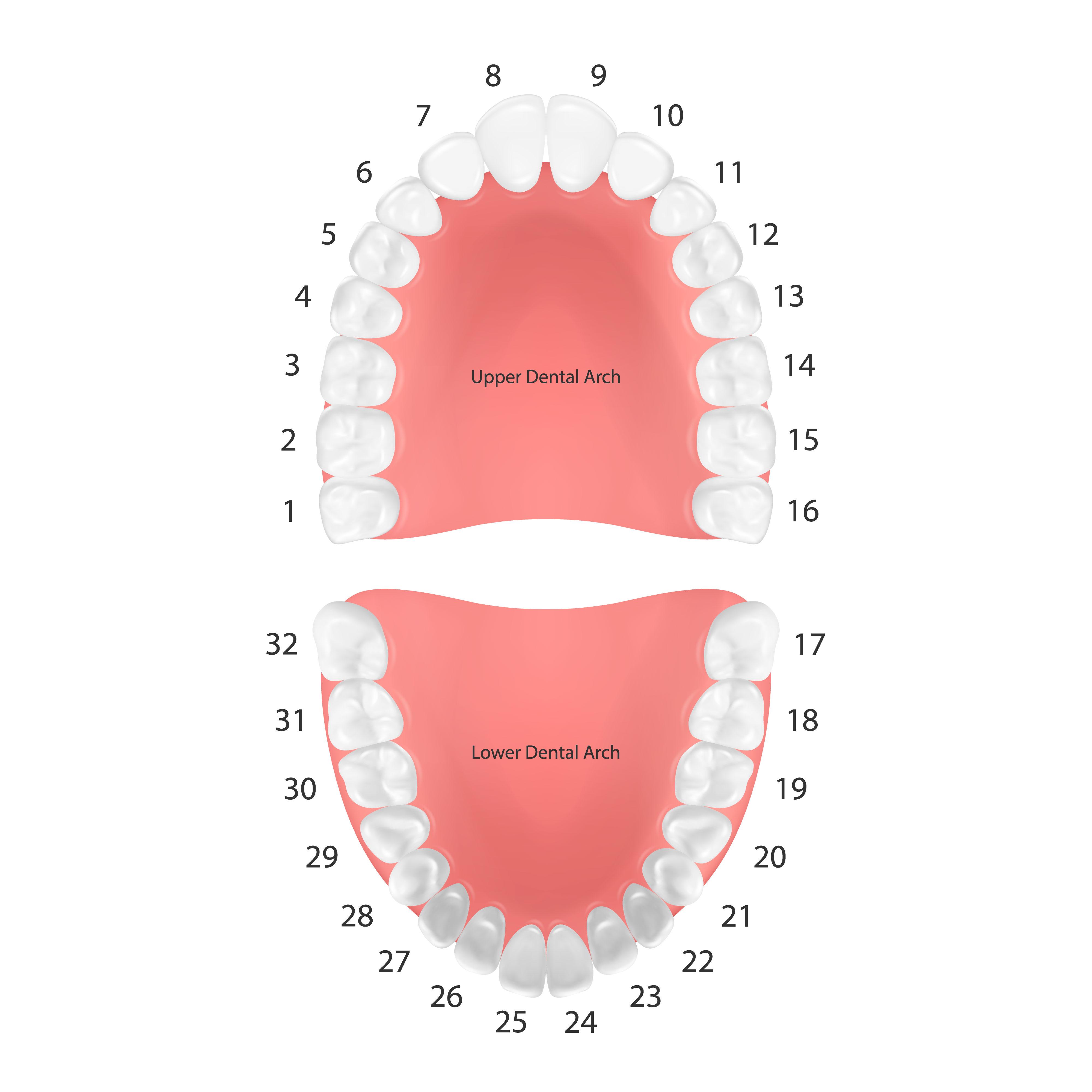 |
Source: Getty Images |
Periodontal disease has been linked to cardiovascular disease, diabetes, and stroke, underscoring the importance of integrating oral health into the patient examination. National Institutes of Health research highlights that oral disease can adversely affect nutrition, speech, psychosocial well-being, and overall quality of life.2,4,5
Primary care physicians should:
- Conduct thorough oral examinations as part of every physical assessment.
- Identify risk factors for oral disease and implement preventive measures.
- Recognize conditions requiring referral to general dentists or dental specialists.
- Understand the systemic implications of oral health disorders.
By strengthening collaboration between primary care, dentistry, and oral surgery, clinicians can bridge current gaps in knowledge and ensure comprehensive patient care.
Conducting the Oral Examination
A successful oral examination begins with establishing a calm, distraction-free setting that promotes patient comfort and trust. Clear communication of instructions is essential, and patients should be given the opportunity to ask questions or request clarification.1
Following the oral examination by the provider, offering clear, constructive feedback is essential. This discussion should outline normal findings, highlight areas of concern, and explain their potential implications. Such dialogue promotes patient understanding, engagement, and adherence to follow-up care.1
Oral Health Conditions
Oral Lichen Planus
Oral lichen planus is recognized as a chronic inflammatory condition that affects the mucous membranes of the oral mucosa. It is demonstrated as a characteristic white, lacy pattern on the tongue, cheeks, gums, and other areas of the mouth.2,3 (See Figure 2.)
Figure 2. Oral Lichen Planus |
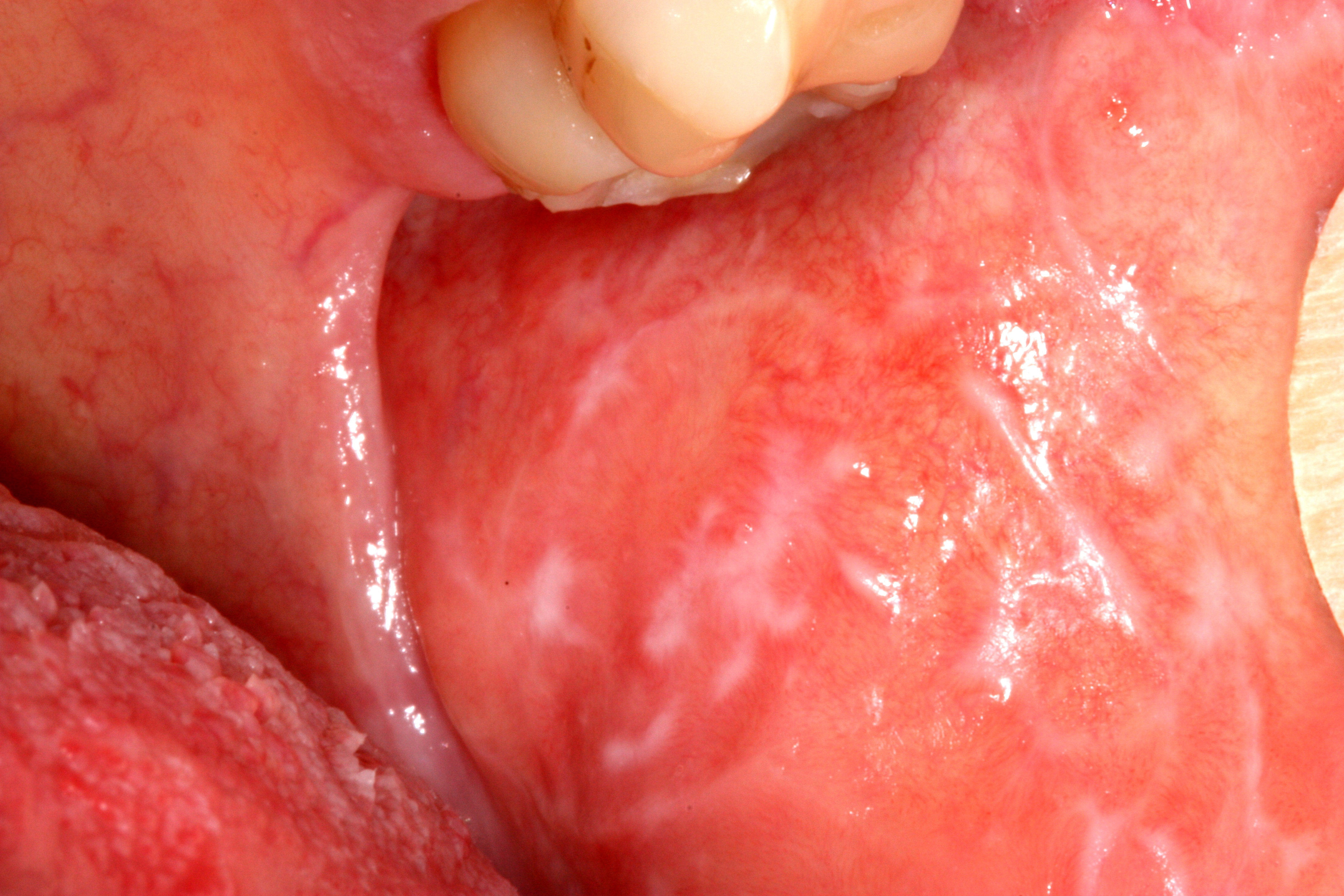 |
Classic white striations of non-erosive lichen planus in the left buccal mucosa (left cheek) |
Source: Ian Furst. https://creativecommons.org/licenses/by-sa/4.0/deed.en |
The symptoms are viewed as white or grayish-white lacy patches, often showing redness and swelling, as well as ulcers or sores. Oral burning or pain when eating or drinking as well as sensitivity to hot or spicy foods also are experienced.
The exact cause of oral lichen planus is unknown, but it is believed to be an autoimmune disorder. Factors that may trigger or worsen the condition are medications, dental procedures, and allergies.6,7
The treatment for oral lichen planus consists of managing the symptoms and preventing complications. Options can include topical corticosteroids (creams or rinses), oral medications (such as antihistamines or immunosuppressants), and changes in lifestyle (such as avoiding triggers and managing stress).6,7
Even though oral lichen planus is described as a chronic condition, it usually does not lead to serious complications. Most cases of oral lichen planus resolve on their own, often within a few years, although some may persist indefinitely. Some cases may lead to squamous cell carcinoma.6,7
An important note regarding oral lichen planus is that it is not contagious. Although more common in women than in men, it is demonstrated in both sexes. Other areas of the body, such as the skin and nails, also can be affected. It is important to refer the patient to a dentist or ear, nose, and throat (ENT) physician if you suspect oral lichen planus.6,7
Oral Leukoplakia
Oral leukoplakia can appear as red, white, or gray patches in the oral cavity and cannot be scraped off (see Figure 3). The patches can be thick, flat, or even slightly raised, and also might have an irregular shape. These patches also can be seen as smooth, rough, fuzzy, or ridged in nature.6,7
Figure 3. Oral Leukoplakia |
 |
Photo taken of patient, who will remain anonymous, treated at the University of Tennessee Health Science Center College of Dentistry in Memphis, TN. The lesion is an example of leukoplakia. Biopsy was going to be done later to establish a specific diagnosis. |
Source: Michael Gaither. https://creativecommons.org/licenses/by-sa/3.0/deed.en |
Located on the gums, the inside of the cheeks, the bottom of the mouth, or tongue, the patches usually are painless but may be sensitive to touch, heat, or other irritation.6,7 Sometimes these patches can be sensitive or even painful when they come into contact with acidic or spicy food.
Leukoplakia can be a sign of oral cancer or a precancerous lesion. Treatment involves removing the patches with a laser or scalpel. The area should be numbed with a local anesthetic or general anesthesia. The mouth should heal quickly, and follow-up visits should be scheduled to monitor the healing process.6,7
Treatment for leukoplakia is most successful after a patch is discovered and receives early treatment when it is small. The patient’s mouth should be checked regularly for changes to the cheeks, gums, and tongue.6,7
Stopping the source of irritation (such as tobacco or alcohol use) often clears the condition. If lifestyle changes do not work or early signs of cancer are observed, the patches may be removed using a small surgical knife, laser tool, or cryotherapy to destroy the cancer cells. A referral to an ENT specialist is indicated if the primary care physician is not familiar with the procedure.2,8
Black Hairy Tongue
Black hairy tongue is a benign oral condition presenting as an overgrowth of elongated, pigmented filiform papillae on the dorsal surface of the tongue (see Figure 4). This exhibits as a black or dark brown hairy or furry appearance on the tongue. Black hairy tongue most often is caused by poor oral hygiene, smoking, or the use of certain medications (e.g., antibiotics or antihistamines). Heavy consumption of coffee, tea, or dark-colored foods also can contribute to the condition. A yeast overgrowth also may be present, as well as an unpleasant taste or bad breath. Diagnosis most often is made by visual examination. The patient can mitigate the condition by improving their oral hygiene by brushing and flossing regularly. The use of an antifungal mouthwash or toothpaste and, in some situations, the use of topical medications or laser therapy, also may be employed.2,6-8
Figure 4. Black Hairy Tongue |
 |
Lingua villosa nigra associated with chromogenic organisms (e.g., C. albicans) and certain medications (doxycycline and bismuth) |
Source: Com4. https://commons.wikimedia.org/wiki/File:Black_tongue.jpg |
The condition usually is self-limiting and will resolve with improved oral hygiene. However, it may, in some cases, persist or recur. Black hairy tongue is not contagious and often is associated with conditions such as dry mouth (xerostomia) or the natural shedding of keratin. Dehydration also can be responsible for the condition, as well as not eating or eating only soft foods. Most people with black hairy tongue have no symptoms whatsoever other than some cosmetic concerns. Long papillae also can cause pain and bleeding if picked at. Drinking water and staying hydrated, as well as limiting caffeinated beverages and eating a balanced diet, also can help.6,7,9
Oral Syphilis
Syphilis is an infectious disease caused by Treponema pallidum. Syphilis may be transmitted from mother to child, although the infection largely is spread through direct contact with a lesion. It can be transmitted through oral, vaginal, or anal sex. For purposes of this review, the focus will be on oral sex.6,7,10
In 2001, the incidence of syphilitic infections was the lowest reported since 1941; unfortunately, cases of syphilis have increased in recent years.6,7,10
Humans are the only natural host for syphilis. Re-infection of the host is possible. Primary, secondary, and tertiary syphilis all can be present with oral manifestations (see Figure 5). Oral manifestations often are the first sign of infection. Syphilis is curable with the use of antibiotics, but many cases go undiagnosed. If unrecognized, it can reach the tertiary stage, which may lead to fatal neurologic and cardiovascular diseases. Prompt awareness of the clinical features is imperative. Early identification of the oral manifestations, followed by a biopsy, will prove useful in treating the resurgence of syphilis.6,7,10
Figure 5. Oral Syphilis |
 |
Primary stage syphilis sore (chancre) on the surface of a tongue |
Source: Centers for Disease Control and Prevention. https://www.cdc.gov/syphilis/hcp/images/index.html |
For clinicians, the importance of identifying the oral manifestations of syphilis cannot be understated. Syphilis has been referred to as the great imitator, since its signs, symptoms, and presentation depend largely on the age of the lesion. Referral to an oral pathologist may be indicated. Because of the inflammatory processes of the mouth, the clinical correlation often is salient for proper diagnosis of the biopsy.6,7,10
Angular Cheilitis
Angular cheilitis is a common, non-contagious, inflammatory condition that affects the corners of the mouth or oral commissures with oozing, crusting, and redness (see Figure 6). Most often it is seen bilaterally as gray macerations at the corners of the mouth. It may last a few days or persist indefinitely. It also may be referred to as angular stomatitis, cheilosis, rhagades, or perleche. Many edentulous patients or patients who wear dentures often present with angular cheilitis because of the loss of vertical dimension.6,7
Figure 6. Angular Cheilitis |
 |
Photograph of bilateral angular cheilitis in an elderly individual with false teeth, iron deficiency anemia, and xerostomia |
Source: Matthew Ferguson 57. https://creativecommons.org/licenses/by-sa/3.0/deed.en |
Angular cheilitis is common and can affect both children and adults. Those with poor health are especially susceptible to angular cheilitis. It most often is caused by prolonged exposure of the corners of the mouth to saliva and its digestive enzymes. As with most oral conditions, lack of good nutrition as well as smoking can contribute to angular cheilitis. Also, iron, riboflavin, protein, zinc, and vitamin B12 deficiency can be linked to angular cheilitis.6,7
In the early stages of cheilitis, changes may be more subtle in patients with darker skin. Even if left untreated, angular cheilitis seldom causes permanent scarring and discoloration of the skin. If the corners of the mouth are swabbed and cultured for Candida albicans, Staphylococcus aureus, or herpes simplex virus, angular cheilitis most often is diagnosed by patient history and clinical examination.6-8
In most cases, no treatment is needed for angular cheilitis, and it will resolve on its own, usually within two weeks. To help resolve cheilitis, better hydration, use of lip balm, and topical antiseptics are indicated.6,7
Ranula
A ranula presents as a fluid-filled cyst forming under the tongue, usually in the sublingual land (see Figure 7). It typically is a painless lump. A ranula usually is caused by a blocked salivary gland that becomes infected, although there may be other unknown causes. It also may appear white or bluish in color and cause difficulty in speaking, eating, or swallowing. A ranula usually is found during an oral examination by a dentist or physician and often requires a biopsy if there is a suspicion of cancer. Often, a small ranula may resolve itself gradually on its own.1,6,7,10
Figure 7. Ranula |
 |
Source: Ph0t0happy. https://creativecommons.org/licenses/by-sa/3.0/deed.en |
Usually, the cyst and affected sublingual gland are surgically removed. A marsupialization procedure also can be performed, in which the cyst is opened and the edges are stitched to the inside of the mouth. This procedure allows it to drain. Most ranulas are successfully treated with conservative measures or surgery, and recurrence is less common after surgical removal. Ranulas are not contagious and are more common in children and young adults. The patient should avoid biting or puncturing a ranula, since this can lead to an infection. A ranula seldom goes away on its own untreated.6,7,10
Acute Necrotizing Ulcerative Gingivitis
Acute necrotizing ulcerative gingivitis (ANUG) is a gingival infection that causes painful inflammation and ulceration (see Figure 8). It also is known as trench mouth or Vincent’s gingivitis.6,7
Figure 8. Acute Necrotizing Ulcerative Gingivitis |
 |
Source: Getty Images |
Generally, it is first noticed by the patient as being painful and inflamed, with crater-like lesions in the gingiva accompanied by fever and bad breath, as well as a metallic taste and a feeling of illness. The patient may complain of loose teeth as well.
ANUG is caused by an overgrowth of normal bacteria in the mouth. Also, an impaired immune response may be present. It may be treated with antibiotics, periodontal cleaning, and saltwater or hydrogen peroxide rinses. The patient should avoid hot and spicy foods. Eating a balanced diet is essential. Risk factors include smoking, poor oral hygiene, malnutrition, and human immunodeficiency virus (HIV) infection. ANUG was common in the military during World War I, but it is less common now in the general population.6,7
Generalized Periodontal Disease
Generalized periodontitis is a severe form of gum disease that affects multiple teeth and is treated with deep scaling and root planing (see Figure 9). It presents as rapid progression of periodontal tissue destruction, which leads to tooth loss if not treated.
Figure 9. Generalized Periodontal Disease |
 |
Clinical and radiographic example of periodontal disease |
Source: DRosenbach. https://creativecommons.org/licenses/by-sa/4.0/deed.en |
Generalized periodontal disease is caused by a bacterial infection (primarily anaerobic bacteria), hormonal changes (e.g., pregnancy, menopause, genetics), smoking, and diabetes. The patient presents with red, swollen, bleeding, and tender gums. On examination, the patient will have periodontal pockets in excess of 5 mm. The gingiva may bleed, especially when brushing or flossing. The patient may complain of bad breath and loose teeth. A referral to a dentist or dental hygienist is indicated for X-rays and comprehensive dental cleaning.
Antibiotic therapy, as well as scaling and root planing by a hygienist or periodontist, or periodontal surgery by the periodontist, generally is indicated. Lifestyle changes (e.g., smoking cessation, improved oral hygiene, healthier diet, and regular dental check-ups) are necessary to prevent periodontal disease from recurring. If not treated, periodontal disease can lead to tooth and bone loss and an increased risk of heart disease and stroke.2,4,5
Periodontal Disease and Systemic Heart Disease
Periodontal disease, also known as gum disease, can be linked to an increased risk of systemic heart disease. This is the result of a combination of factors, including inflammation, bacteria, and other shared risk factors. Periodontal disease is a bacterial infection that triggers chronic inflammation in the gums and the body. It can contribute to the development of atherosclerosis, where dental plaque can build up in the arteries, potentially leading to heart disease. The oral bacteria that are associated with periodontal disease can enter the bloodstream and can cause infections in the heart valves and contribute to the formation of blood clots in the arteries. Other risk factors for heart disease, such as smoking, unhealthy diets, and lack of exercise, can further increase the risk. Some studies have shown that people with periodontal disease may be at a two to three times greater risk of having a heart attack or other cardiovascular problems. Treating periodontitis may help improve these cardiovascular risk factors.2,4,5
Canker Sores
Canker sores do not need testing to diagnose. The primary care physician can identify canker sores with a visual examination (see Figure 10). The provider may want to check for other health problems if the canker sores are severe and ongoing.8
Figure 10. Canker Sore |
 |
Source: Maksim. https://creativecommons.org/licenses/by-sa/4.0/deed.en |
Minor canker sores will resolve in one to two weeks. Large, persistent, or unusually painful sores often require medical care. There are several options available, such as mouth rinses containing the steroid dexamethasone, which help to reduce pain and inflammation.8
Over-the-counter and prescription medications, such as pastes, creams, gels, or liquids, also may help to relieve pain. If applied to individual sores as soon as they appear, these also may assist in healing. Some products contain active ingredients such as benzocaine (Anbesol, Kank-A, Orabase, Zilactin-B), fluocinonide (Lidex, Vanos), or hydrogen peroxide (Orajel, Colgate Peroxyl). Medications that are not specifically intended for canker sores, such as the intestinal ulcer treatment sucralfate (Carafate) used as a coating agent and colchicine that normally is used to treat gout, also can be used. Treatment also can consist of cautery to burn or sear the tissue.8
By using sulfonated phenolics/sulfuric acid (Debacterol), a topical solution to treat canker sores and gum problems, the healing period may be reduced by about a week. A nutritional supplement such as folate (folic acid), vitamin B6, vitamin B12, or zinc in reduced amounts also can shorten healing time.8
Oral Thrush
Oral thrush, also known as oral candidiasis, is a fungal infection of the mouth. It is caused by the Candida albicans yeast. Thrush appears as creamy white patches on the tongue, inner cheeks, roof of the mouth, or gums (see Figure 11). Oral thrush also may spread to the tonsils or back of the throat. Oral thrush can appear as raised patches resembling cottage cheese. Even though thrush can be wiped off, red areas remain.8
Figure 11. Oral Thrush |
 |
This image depicts a condition known as oral thrush, which manifested as a result of a Candida albicans infection. Note the yellowish-beige colored oral ulcers known as aphthae. |
Source: Centers for Disease Control and Prevention Public Health Image Library |
Thrush produces soreness or a burning sensation in the mouth. This is felt especially when eating or drinking. There can be an unpleasant taste in the mouth. Redness and inflammation of the mouth lining also can be observed, with dryness and cracking at the corners of the mouth. In severe cases of thrush, there also can be difficulty in swallowing. Sometimes there is a feeling of thickness or “cotton” in the mouth. A patient with oral thrush may not experience all of these symptoms.8
Oral thrush can affect anyone, but it is more likely to be found in babies and older adults because they have lower immunity. It may be diagnosed in other people with weakened immune systems or certain health conditions, or people taking certain medicines. Oral thrush is a minor problem if the patient is healthy, but in those with a weakened immune system, the symptoms may be more serious and more difficult to control.8
Redness, burning, or soreness may be serious enough to cause difficulty eating or swallowing. There can be slight bleeding if the patches or spots are rubbed or scraped. In addition to cracking and redness at the corners of the mouth, the patient may have a loss of taste.
Denture wearers may present with redness, irritation, and pain under their dentures. The patches or spots may spread downward into the esophagus in severe cases when related to cancer or a weakened immune system from HIV/acquired immunodeficiency syndrome (AIDS). This is called Candida esophagitis. When this occurs, the patient may have difficulty eating and swallowing.8
In addition to the distinctive white patches, babies may have trouble feeding or become fussy and irritable. The infection can be transmitted to mothers during breastfeeding. The infection may pass back and forth between the mother’s nipples and the baby’s mouth.8
Women whose breasts are infected with Candida usually present with red, sensitive, cracked, or itchy nipples. The areola may be shiny or flaky. The breastfeeding mother also may feel stabbing pains within the breast. Thrush is not normally found in healthy children, teenagers, and adults. If such a patient presents with thrush, they should be checked for any underlying medical condition or another cause.8
Several medications can increase the risk of developing oral thrush as the result of disrupting the natural balance of microorganisms in the mouth. These include antibiotics, inhaled corticosteroids, and some medications that cause dry mouth.8
Geographic Tongue
Geographic tongue, or benign migratory glossitis, is a chronic condition causing smooth, red patches to appear on the tongue (see Figure 12). These red patches move around on the surface of the tongue, changing their shape and size. They might be mistaken for sores. A burning sensation when eating spicy or acidic foods also can be present. The lymph nodes in the lower jaw also may become swollen. Other areas of the mouth, such as the gums, may show red patches.8
Figure 12. Geographic Tongue |
 |
Source: Martanopue, Jbarta (derivative work). https://creativecommons.org/licenses/by-sa/3.0/deed.en |
The cause of geographic tongue is not known, but it possibly may include vitamin (B6, B12, B9 [folate], D) and mineral (zinc, iron) deficiencies. Psychological factors, as well as emotional stress, also may contribute to geographic tongue. Smoking and alcohol use, as well as allergies and diabetes, also may be responsible for the condition.2,8
Treatment varies, but in rare cases pain relievers and rinses may be used to treat symptoms. Occasionally, geographic tongue becomes self-treatable. A lighted instrument can be used to check the tongue and mouth when diagnosing geographic tongue. The patient should be asked to move their tongue around into various positions. The examiner should touch the patient’s tongue to check for tenderness or changes in the tongue. Some symptoms of geographic tongue may look like other conditions, such as oral lichen planus; these conditions may need to be ruled out before making a definitive diagnosis.6-8
Geographic tongue usually does not require medical treatment. Although geographic tongue sometimes causes pain in the tongue, it is a harmless condition. If medical treatment is indicated, some antibiotic mouth rinses can be used to numb the affected area and reduce swelling. In extreme cases, a corticosteroid ointment or rinse can be used to manage the condition. These treatments have not been studied in great detail; therefore, their benefits are not known.8
Thrush vs. Geographic Tongue
Although both thrush and geographic tongue can appear as patches on the tongue, thrush is fungal and geographic tongue is not. The infection that is caused by Candida yeast (thrush), causing creamy white patches that can be wiped off, is different from geographic tongue, a benign condition presenting with smooth, red patches surrounded by white borders that look like a map and is not caused by an infection. Thrush is an infection, while geographic tongue is a harmless variation in tongue appearance and is considered harmless.8
A white tongue often is harmless, but it can point out more serious health conditions, such as lichen planus or oral leukoplakia. Other conditions that mimic oral thrush are less serious, such as geographic tongue, canker sores, coated tongue, and milk tongue.6-8
Milk Tongue vs. Thrush
Common in young babies, a white tongue does not always mean it is thrush. It can be caused by the residue of milk that has been spit up, leaving a condition called milk tongue, and it can be wiped away easily and is not painful.8
Milk tongue is normal and will go away as soon as solid foods become a consistent part of the baby’s diet. The best way to manage a milk tongue is to practice good oral hygiene, including gently wiping the child’s tongue after feeding.8
Maxillary and Mandibular Tori
Although most oral lesions are soft, torus palatinus and torus mandibularis develop, respectively, as cortical, osseous outgrowths from the midline of the palate and the inner surface of the mandible (see Figure 13). They start forming during puberty and grow into adulthood. Tori rarely cause pain or other symptoms except when they interfere with a comfortable fit of an oral appliance, such as a complete or partial denture, or mastication trauma from chewing hard foods.
Figure 13. Maxillary and Mandibular Tori |
 |
Maxillary tori |
Source: Kozlovsk. https://creativecommons.org/licenses/by-sa/3.0/deed.en |
 |
Right mandibular torus |
Source: DRosenbach. https://creativecommons.org/licenses/by-sa/3.0/deed.en |
Although oral bony tori usually are harmless and do not require removal, they should be considered for removal if they become uncomfortable or painful. As mentioned earlier, they can interfere with eating as well as with speaking. The main causes of oral tori removal are inflammation, food impaction, and the placement of a removable prothesis. Surgery should be performed by a dentist or oral surgeon. A laser often is used.
Factors that can cause the development of oral tori include genetics, grinding teeth, jaw clenching, and injury to the jaw or head.
Rampant Dental Caries
Rampant tooth decay is a condition in which multiple teeth have generalized and rapidly growing cavities (see Figure 14). It also can be referred to as severe tooth decay.6,7
Figure 14. Dental Caries |
 |
Class 5 cavities on the upper teeth |
Source: Ickyvickywiki. https://creativecommons.org/licenses/by-sa/4.0/deed.en |
The main cause is not brushing or flossing on a routine basis. High sugar consumption, including sodas, sports drinks, and candy, contribute significantly to severe tooth decay. Some medications can cause dry mouth (xerostomia), that can lead to tooth decay. Radiation therapy to the head and neck also can cause tooth decay.6,7,9
Severe tooth decay can produce discomfort, sensitivity, and pain. If teeth are not treated with endodontics, the pulp chamber becomes infected and an abscess forms. This contributes to tooth loss and decreased function. This can be treated by referring the patient to a dentist or endodontist who will remove the diseased portion of the tooth pulp, placing a material in the pulp chamber and thus save the tooth for further treatment.6,7
When the patient presents with rampant caries, they should be counseled to practice good oral hygiene, including brushing and flossing. Brushing should be in a circular motion with the brush pointed at a 45-degree angle toward the gums for a minimum of three minutes (Bass technique), at least twice per day. The patient also should use their toothbrush to massage their gums. The palate and tongue also should be cleansed. The patient’s toothbrush should be thoroughly rinsed and placed in an upright position.6,7
In recent years, a rotary toothbrush has been proven to clean up to 20% better than a manual one. The head of the rotary toothbrush should be replaced every three months. Even though flossing is recommended daily, care should be exercised not to damage the tissue.
Rinsing the mouth with an antiseptic mouthwash (Listerine, Colgate Pro-Health, Act) will help to improve the patient’s overall oral health. An acidic mouth will demineralize the pores in the tooth enamel, causing decay to begin and spread throughout the dentition.
Another cause of severe tooth decay is stomach acid reflux. The primary care provider should recommend to the patient that it can be controlled by medication and other adjunctive saliva substitutes (Biotene), and certain chewing gums that stimulate saliva production, mouth sprays, and toothpastes.6,7,9
Adequate salivary flow is necessary for reducing acid in the mouth. Without this normal flow of saliva, the patient’s teeth are more susceptible to rampant decay. The patient may develop dry mouth (xerostomia), which makes it more difficult to treat. This can be caused by factors such as salivary glands damaged by trauma and disease. Also, medications the patient is taking for depression, anxiety, obesity, pain (opioids), epilepsy, high blood pressure, and psychotic disorders can influence and slow the patient’s saliva flow. When a patient presents for an examination with a water bottle, it might not be only for good hydration.9
If possible, stop or change medications causing salivary issues. Having a patient in a stable condition with no infection or tooth decay is ideal. For patients with dental caries, referral to a dentist is always indicated. Dental treatment can be completed in phases by restoring the most immediate concerns first but still bringing the patient into good oral health.
Dental caries is treated with restorative materials that include replacing much of the tooth that presents with rampant decay. The best course of action is always to advise the patient that prevention is necessary. Advise the patient maintaining a good oral care routine by brushing their teeth twice per day with fluoride toothpaste and flossing set the patient up for success. Dental caries has a significant effect on overall health and, untreated, can lead to pain, infections, and systemic diseases, affecting the patient’s quality of life and productivity.
Dry Mouth and its Relation to Scleroderma
Dry mouth (xerostomia) is a common symptom in people with scleroderma, an autoimmune disease that causes skin and tissue hardening. Up to 70% of scleroderma patients experience dry mouth as the result of fibrosis (scarring) of the salivary glands, which can lead to reduced saliva production. This, in turn, can cause difficulty with swallowing, taste, and speech, as well as increase the risk of gum disease and cavities. Although dry mouth can be a challenging symptom, there are strategies to manage it, such as staying hydrated to help keep the mouth moist. Sugar-free chewing gum can stimulate saliva production, and over-the-counter products such as Biotene mouthwash and oral gel can provide relief. In some cases, prescription medications may be recommended to increase saliva production. Regular dental check-ups are important for monitoring and addressing oral health problems.2,9
When it comes to oral manifestations, stopping smoking probably is the most important. Mark Twain once said, “It is easy to stop smoking. I’ve done it a thousand times.” Another habit to be avoided or limited is alcohol consumption.2,8
Staying well-hydrated also is essential; drinking up to eight glasses of water per day is recommended. The patient should practice good oral hygiene and be referred to a dentist for regular check-ups. The patient should be encouraged to brush their teeth at least twice per day after meals with a soft toothbrush and a mild fluoride toothpaste that does not contain sodium lauryl sulfate. Flossing at least once per day followed by an alcohol-free mouthwash also should be recommended. Although not usually practiced, brushing or using a tongue scraper also is encouraged.2,8
A healthy diet that includes plenty of fruit and vegetables also should be encouraged. Avoid or limit food and drinks that are spicy, salty, acidic, or are very hot. All of these can irritate the patient’s mouth.
The Use of Supplemental Fluoride
Supplemental fluoride, in the form of tablets, drops, or vitamin-fluoride combinations, is recommended to help prevent cavities. This is especially important in children who do not have access to fluoridated water. It also helps to strengthen enamel as it develops, thus making teeth more resistant to acid breakdown. However, it is extremely important to use it properly to avoid dental fluorosis. Fluoride supplements should be prescribed to provide both systemic and topical benefits in developing and erupted teeth.
The American Dental Association (ADA) and other health organizations recommend fluoride supplements for children who do not have access to optimally fluoridated water (0.7 ppm, or 0.7 mg/L, fluoride) and are at high risk of developing dental cavities. Fluoride helps prevent cavities by combining with developing enamel, thus making teeth more resistant to acids in the mouth. Supplements are prescribed in liquid, tablet, or lozenge form and the dosage schedule depends on the age of the child. It is very important to follow the recommended dosage to avoid potential side effects, such as enamel fluorosis, which can cause discoloration or mottling of the teeth.
Parents and caregivers should consult with their family dentist, pediatrician, or physician to determine if their child needs fluoride supplements and to discuss the appropriate dosage and use.
Misalignment Options and Approximate Costs for Treatment
Straightening teeth can be accomplished using various options. This includes traditional braces, clear aligners, and lingual braces. The cost of these treatments varies, with braces typically ranging from $3,000 to $10,000, and clear aligners averaging between $2,500 and $8,000. Traditional metal braces still are a common and effective way to correct misaligned teeth. Brackets and wires are attached to the teeth to gradually move them into the proper position. Less visible options include ceramic braces that are tooth-colored or clear brackets. Lingual braces are placed on the lingual side of the teeth, making them practically invisible to others. Clear aligners are removable trays to be worn over the teeth to gradually expand the arch and straighten the teeth.11,12
Some orthodontists offer shorter treatment for cosmetic straightening, focusing on the front teeth. Retainers are used after treatment is accomplished to maintain the correct position of the teeth. Retainers can cost from $100 to $500. The final cost will depend on factors such as the severity of the misalignment, the chosen treatment method, the orthodontist’s fees, and insurance coverage.11,12
The Role of Flossing and Water Flossers
Flossing and water flossers (such as Waterpik) both play important roles in maintaining good oral hygiene by removing plaque and debris between teeth and along the gum line. Flossing removes plaque and food particles from tight spaces in between the teeth where a toothbrush cannot reach. Its use involves gently sliding the dental floss between the teeth to remove plaque and debris. It contributes to healthy gums by reducing gum bleeding and lowering the risk of gum disease. It does require some manual dexterity, which may be difficult for some individuals.13
Water flossers rinse away food particles, plaque, and bacteria from in between teeth below the gingiva. This is accomplished by using a stream of pressurized water to flush out bacteria and debris that may be missed with traditional flossing. This application also is good for cleaning between tightly spaced teeth and cleaning around dental implants, bridges, and crowns, as well as improving gingival health. Although both flossing and water flossers are effective at removing plaque and debris, they offer different cleaning capabilities and often are best used in combination for comprehensive oral health.13
The Role of Coffee, Tea, Alcohol, and Cola Drinks on Dental Health
Coffee, tea, alcohol, and soda can negatively affect dental health by causing tooth stains, and enamel erosion, and increasing the risk of cavities. Acidity and sugar can erode tooth enamel and cause plaque to form that results in decay if not removed thoroughly each day. Many beverages, including coffee, tea, and soda, are very acidic, causing tooth enamel to dissolve. The protective enamel outer layer of the teeth then becomes more susceptible to cavities and more sensitive.2,8
Sugary drinks, such as soda and some alcoholic beverages, provide additional and concentrated bacteria in the mouth. These bacteria produce acids and give off an endotoxin that further damages the enamel, which contributes to an increase in tooth decay and gingivitis. Coffee and tea (especially black tea) can stain the teeth because of color pigments such as tannic acid. Alcohol, particularly red and dark wines, also causes teeth to stain because of their chromogens, and also can dry out the mouth, causing xerostomia, reducing saliva production. Saliva is essential for removing bacteria and plaque. It is difficult to eliminate these various beverages entirely, but moderation is key. Brushing twice per day after morning and evening meals, drinking water after consuming acidic or sugary beverages, and using a straw to decrease contact with the teeth can help to reduce negative effects. Periodic dental check-ups and cleanings also are necessary to maintain optimal dental health.2,8,9
Dental X-Rays: Frequency and Type
The frequency and type of dental X-rays depend on individual needs, with general guidelines varying based on age, oral health, and risk factors (see Table 1). For adults with healthy teeth, bitewing X-rays every 18-36 months are typical, but more frequent X-rays may be needed for children, or those with a history of decay, or those with specific dental conditions.
Table 1. General Dental X-Ray Guidelines |
Healthy adults
Children
Individuals with high risk factors (e.g., extensive decay, gum disease, smoking)
|
Periapical X-rays show the entire tooth, from the crown to the root, and can diagnose issues such as abscesses, cysts, or impacted teeth (see Figure 15). Bitewing X-rays are used to detect cavities between teeth, to evaluate the health of the teeth and gingiva, and to evaluate periodontal bone loss caused by gingival disease (see Figure 16). Panoramic X-rays provide a broad view of the entire mouth, useful for assessing the position of teeth, especially wisdom teeth, and detecting tumors or other abnormalities (see Figure 17).
Figure 15. Periapical X-Ray |
 |
Periapical X-ray: Dental radiograph showing bone loss in a patient who consumes two packs of cigarettes. |
Source: Shaimaa Abdellatif. https://creativecommons.org/licenses/by-sa/4.0/deed.en |
Figure 16. Bitewing X-Ray |
 |
Intraoral bitewing radiograph; this film shows left side healthy dentition, no dental caries |
Source: Source: DRosenbach. https://creativecommons.org/licenses/by-sa/3.0/deed.en |
Figure 17. Panoramic X-Ray |
 |
Source: Getty Images |
Cone beam computed tomography (CBCT) is a 3D imaging technique that provides detailed views of bone and soft tissues, helpful for complex cases and implant planning. Children and teenagers require more frequent X-rays to monitor tooth development. A history of extensive decay, gum disease, or other dental issues may necessitate more frequent X-rays. Factors such as smoking, dry mouth, or diabetes can increase the risk of oral health problems, potentially requiring more frequent X-rays. The frequency and type of dental X-rays depends on individual needs, with general guidelines varying based on age, oral health, and risk factors.
Teeth Whitening Agents: What Are the Options?
Teeth whitening agents, such as hydrogen peroxide and carbamide peroxide, are commonly used to whiten teeth, but the frequency of use should be considered to avoid enamel damage and sensitivity. Professional whitening typically is recommended once or twice per year, while at-home whitening kits can be used for maintenance every three to six months. Hydrogen peroxide is a powerful bleaching agent that is used in professional whitening treatments and at-home kits. At-home whitening kits can be used for initial whitening for up to 14 days or, as noted earlier, for maintenance every three to six months. Over-the-counter products are best for touch-ups and maintaining results, but not for daily use. Professional treatments are more effective and longer lasting, requiring less frequent use. If the patient has sensitive teeth, whitening too frequently can cause discomfort, requiring less frequent treatments. Habits such as smoking and consuming staining foods can affect the longevity of whitening results, requiring more frequent treatments. Proper brushing and flossing can help maintain whiteness for longer, reducing the need for frequent whitening treatments.4,5
Oral Health and Cardiovascular Disease
As mentioned earlier, research has shown that there is a strong connection between oral diseases, particularly periodontitis, and cardiovascular disease. Chronic inflammation from the bacteria in the oral cavity can contribute to and produce atherosclerosis. This is a significant factor in heart disease, and this connection increases the risk of the oral bacteria entering the bloodstream and triggering an inflammatory response, damaging the lining of the blood vessels. This increases the risk of heart attack or stroke.2,4,5
Both oral disease (periodontitis) and cardiovascular disease can share commonality in inducing chronic inflammation and can trigger inflammatory responses systemically. When gums become inflamed, oral bacteria enter the bloodstream and travel to the arteries, forming plaque and damaging the blood vessels.
Summary
The oral cavity lies at the intersection of medicine and dentistry and serves as a critical indicator of overall health. The pathological conditions often exert a more profound effect on systemic health than is commonly acknowledged by many healthcare providers. Ignoring oral health not only exacerbates localized issues but also influences chronic diseases. By being proactive and managing oral health through regular primary care and dental examinations and by maintaining proper oral hygiene, the prevention and management of chronic diseases can be realized. This reduces the incidence of problems associated with poor oral health and decreases mortality rates connected with poor dental and oral health.
Because of limited access to proper medical resources and dental care, many patients do not recognize the onset of more severe health events. This only leads to delays in treatment. It is very important to look further into this issue to increase the awareness of the critical role that oral health plays in the development of chronic diseases and to identify their significance in the prevention and management of systemic conditions.
For physician examinations, understanding the importance of dental health involves recognizing the mouth as a “window” to overall health, with oral health being a key indicator of systemic well-being. A concise oral examination can reveal potential signs of diseases such as diabetes, HIV, and Sjögren’s syndrome. Physicians should be aware of normal variations in oral anatomy and pigmentation to avoid misdiagnoses.
Key Takeaways for the Primary Care Physician
- Oral health as an indicator of systemic health: The mouth can reveal early signs of systemic diseases, making it a valuable tool for early detection and intervention.
- The importance of oral hygiene and preventive care: Encouraging regular dental visits, proper brushing and flossing, and reducing tobacco and alcohol use can improve overall health significantly.
- Recognizing normal variations: Primary care physicians should be aware of normal anatomical variations in the mouth, especially in patients with darker skin, to avoid incorrect diagnoses.
- Cancer screening: Oral examinations can help identify potential signs of oral cancer.
- Effect on other systems: Poor oral health can affect various bodily systems, including the cardiovascular system.
- Effect on physical fitness: Good oral health can improve nutrition, reduce inflammation, and prevent cardiovascular and respiratory infections, all of which can positively affect physical performance.
Terry Schmunk, DDS, MPH, is a Colonel, U.S. Army (Retired); and Associate, Aspen Dental, Tupelo, MS.
References
1. FDI World Dental Federation. How to practice good oral hygiene. https://www.fdiworlddental.org/how-practice-good-oral-hygiene
2. Zupo R, Castellana F, De Nucci S, et al. Beverages consumption and oral health in the aging population: A systematic review. Front Nutr. 2021;8:762383.
3. Mayo Clinic. Oral health: A window to your overall health. Published March 14, 2024. https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475
4. Penn Dental Family Practice. Fact vs. fiction: The gum disease-heart disease myth. University of Pennsylvania. Published July 13, 2023. https://mypenndentist.org/dental-tips/2023/07/13/oral-health-and-heart-disease/
5. Harvard Health Publishing. Gum disease and the connection to heart disease. Harvard Medical School. https://www.health.harvard.edu/diseases-and-conditions/gum-disease-and-the-connection-to-heart-disease
6. Neville BW, Damm DD, Allen CM, Chi AC. Oral and Maxillofacial Pathology. 4th ed. Elsevier; 2015.
7. Regezi JA, Sciubba J, Jordan RCK. Oral Pathology: Clinical Pathologic Correlations. 7th ed. Elsevier; 2016.
8. Mayo Clinic. https://www.mayoclinic.org
9. Biotene. Understanding dry mouth. https://www.biotene.com/dry-mouth-health-impacts/understanding-dry-mouth/
10. Edens MH, Khaled Y, Napenas JJ. Introduction to oral manifestations of systemic diseases: Evaluation of the patient. Atlas Oral Maxillofac Surg Clin North Am. 2017;25(2):85-92.
11. North Coast Orthodontics. Orthodontics. https://northcoastortho.com/lp/orthodontics/
12. NewSmile. https://newsmilelife.com
13. Progressive Periodontics. Water pick vs flossing: Should I use one or the other? Or both! Published March 8, 2021. https://www.myperiopro.com/waterpik-vs-flossing-should-i-use-one-or-the-oth/