
Mass Casualty Incidents
May 1, 2025
By Ellie Ganz, MD; Nicole T. McAllister, DO, MA; and Whitney Briggs, DO
EXECUTIVE SUMMARY
- Traffic accidents seem to be relatively common small-scale mass casualty incidents (MCIs). According to a study using the National EMS Database, 62.7% of MCI-related injuries were due to motor vehicle crashes, with a notable incidence in urban settings and on highways.
- The first class is called “multiple casualties” in which resources are stretched but not exceeded, the threat is controlled, and patients can be reached by providers and transported in a reasonable time. The second level is mass casualty (MASCAL) in which resources are exceeded, the threat may be ongoing, there is a slight delay in getting to the scene, and some but not all patients are able to be evacuated. The most serious level is called Ultra-MASCAL in which resources are greatly exceeded, victim totals may exceed greater than 100, the threat is ongoing, there is a large delay in getting to the scene, and there is limited evacuation of victims.
- A common way to prepare for these high-acuity but low-frequency events is through various types of simulation. Simulation and tabletop exercises, where a group of people analyze and discuss hypothetical emergency situations, allow for different institutions to formalize procedures, develop appropriate lines of communication, establish leadership, and identify potential areas for improvement.
- In pediatric MCIs, it has been found that JumpSTART has been faster in triaging patients compared to Sort, Assessment, Life-saving interventions, Treatment and Transport (SALT). Some reasons why pediatric patients need a different triage system is because of anatomic and physiologic differences and inability to follow commands reliably. Having adjustments in the triage system attempts to accommodate for these differences.
Mass casualty incidents (MCIs) are frightening and challenging for both victims and the healthcare professionals who must provide the highest level of care to the most individuals possible, often in uncertain environments. The authors review critical aspects of MCIs and the latest evidence regarding optimal care and management for patients and staff.
— Ann M. Dietrich, MD, Editor
Mass casualty incidents (MCIs) are increasingly common in recent news headlines, with incidents ranging from hurricanes and tornadoes to terrorist attacks and shootings. A deeper understanding of MCIs is crucial to emergency physicians during these critical times. Emergency physicians are key in caring for victims, and often are looked to as leaders during these events.
This paper examines recent articles, trials, and other sources pertaining to MCIs. Triage protocols are discussed at length because of their importance in delivering patients to the right place as soon as possible. Triage and communication are consistently emphasized as some of the most important aspects of an MCI response. Limitations in caring for victims, such as staffing, MCI plans, availability of blood products, and others, are evaluated further as well. Recommendations based on previous incidents also are discussed.
Additionally, the long-term health and emotional effects of MCIs are examined. The strain that MCIs put on communities and their healthcare systems needs to be understood to better prepare for these inevitable events in the future. Learning from the past to better prepare for the future is key in events that are difficult to train for such as MCIs.
Introduction
MCIs can be unpredictable and devastating for the communities they affect. While these incidents often are thought of as large-scale disasters with high numbers of fatalities, smaller events still can have a large impact on the communities in which they occur. The definition of an MCI is “any event that overwhelms the local healthcare system, where the number of casualties vastly exceeds the local resources and capabilities in a short period of time.”1 The definition of MCI encompasses a wide range of incidents. MCIs often are thought to be the rare large-scale disaster that makes national news. However, MCIs encompass smaller and more local disasters, such as tornadoes or fires, that more commonly overwhelm the local resources.
MCIs occur for many reasons and can include both intentional acts of harm and incidental events. They span a wide variety of events, such as premeditated terrorist attacks, failing infrastructure, weather-related disasters, infectious disease outbreaks, and industrial and transportation incidents. Because of the unpredictable nature and diversity of these events, it is difficult for the healthcare system to be prepared for all possible incidents. MCIs may affect different age groups from young children to the geriatric population, with a wide range of environments affecting triage and treatments. In addition, each type of event may result in different injury patterns. Emergency departments handle chaos frequently, but MCIs add an additional layer of turbulence.
Description of MCIs
The disaster cycle consists of four phases: preparation, response, recovery, and mitigation.2 Response plans are constructed during the preparation phase. This consists of the incident command center and roles if a disaster were to occur. It also takes into consideration resources available. It is important that there is some adaptability to the plan because MCIs are unpredictable and variable. An MCI such as an anticipated hurricane gives additional preparation time to modify or adjust the established response plan.3 This contrasts with something such as a terrorist attack that comes suddenly and without warning. However, it is essential to have an established plan for these other events.
During the response phase, the initial plans are followed, and actions are taken to limit destruction and hazards. Depending on the size of the MCI, different state, regional, or national organizations may become involved. The recovery phase has the ultimate goal of getting the community back to its pre-disaster state. This can be challenging, and funding may vary based on where and what has happened. Highly publicized MCIs may get funding initially, but the recovery phase can be a lengthy process even when it is no longer televised or talked about.3
During the mitigation phase, often there is a review of what worked and what did not work with the previous disaster plan and a discussion of what can be done to prevent and/or reduce damage from future disasters.2 It is difficult to measure the effectiveness of a response plan and the changes made during the mitigation phase.3 The mitigation phase can involve local organizations and possibly even statewide, national, or worldwide organizations. This can add another layer of complexity to the mitigation phase and future disaster plans.
MCIs can be categorized in several different ways. They can be differentiated based on the cause or the response, and they range from natural disasters to industrial accidents, terrorist acts, environmental exposures, and disease outbreaks. Because of the variety of etiologies of these incidents, different levels of care and responses may be required and include emergency medical services (EMS) response, police, air and water rescue, HAZMAT, and other specialty services.
Shackelford et al performed a review of the literature from the Department of Defense Trauma Registry and used a classification system to help assist with expected victims, level of injury, and need for response.4 The first class is called “multiple casualties” in which resources are stretched but not exceeded, the threat is controlled, and patients can be reached by providers and transported in a reasonable time. The second level is mass casualty (MASCAL) in which resources are exceeded, the threat may be ongoing, there is a slight delay in getting to the scene, and some but not all patients are able to be evacuated. The most serious level is called Ultra-MASCAL in which resources are greatly exceeded, there may be 100 to more than thousands of victims, the threat is ongoing, there is a large delay in getting to the scene, and there is limited evacuation of victims. Shackelford and colleagues emphasize the “golden hour,” which references the importance of treating and transporting patients within the first hour of the event. See Table 1 for further explanation of the timeline of life-saving interventions.
Table 1. Timeline of Life-Saving Interventions | |
Time | Intervention |
A few minutes |
|
Less than 30 minutes |
|
“Golden hour,” within one hour |
|
Four hours + |
|
Five hours |
|
Chances of survival stabilize after four hours with ongoing care. | |
Adapted from: Shackelford SA, Remley MA, Keenan S, et al. Evidence-based principles of time, triage and treatment: Refining the initial medical response to massive casualty incidents. J Trauma Acute Care Surg. 2022;93(2S Suppl 1):S160-S164. | |
Epidemiology
The year 2023 was the most expensive year for natural disasters on record, consisting of 28 different weather events leading to about 492 deaths.5 These weather events included wildfires, hurricanes, tornadoes, floods, heat waves, and blizzards. These events lead to the loss of housing, infected/contaminated water supply, and decreased resources (which include access to medications, water, and food). There seems to be an increase in these events over recent decades, demonstrated in Figure 1. MCIs secondary to gun violence also are common, with an increase in the last decade. An epidemiologic study conducted in 2024 concluded that the last decade had not only the most shootings but also was the deadliest.6
Figure 1. Month by Month Accumulation of Billion-Dollar Disasters for Each Year |
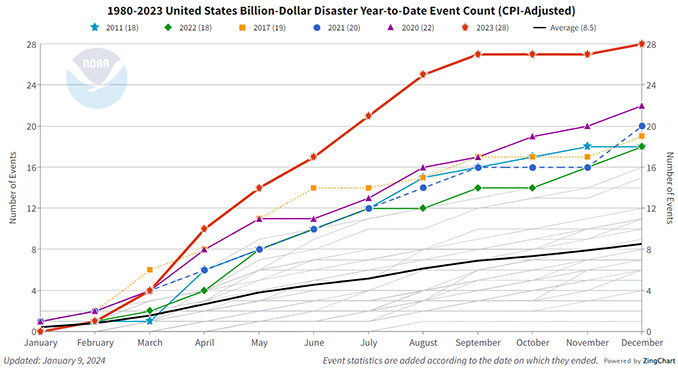 |
Source: Smith A. 2023: A historic year of U.S. billion-dollar weather and climate disasters. Climate.gov. Jan. 8, 2024. https://www.climate.gov/news-features/blogs/beyond-data/2023-historic-year-us-billion-dollar-weather-and-climate-disasters |
In one epidemiologic study performed by Schenk et al, the majority of MCIs occurred in urban settings, during the evening hours, and often on streets or highways.7 Traffic accidents seem to be relatively common small-scale MCIs. According to a study using the National EMS Database, 62.7% of MCI-related injuries were due to motor vehicle crashes, with a notable incidence in urban settings and on highways.7 The South Atlantic region reported the highest frequency of MCIs, despite representing a smaller proportion of the population.
Illness/Injury Patterns
Since there is such a diversity of MCIs, the injury patterns/illnesses also will have a wide variety of presentations.
Some MCIs can involve chemical, radiological, or biological weapons. Decontamination is important after these events for patients, staff, and bystanders. Decontamination helps prevent further injury for the patient and avoid further contamination and future victims.8 Disrobing is an essential first step to the process, followed by gross decontamination. For MCIs, there needs to be a fast and efficient way to do this for large numbers of victims. One method is called the “ladder-pipe system,” which positions ladders and hoses from two or more fire trucks to form a shower corridor for victims to go through.8 This method can be effective, but the concern is the possible delay in decontamination.9 Collins et al encourage taking initial steps, such as disrobing and interim decontamination, before the ladder-pipe system can be set up. It also is important to note that some victims may need additional help during this process if they are unable to ambulate because of their injuries. Communication and collaboration with EMS agencies and hospital systems to establish decontamination sites prior to major incidents are key to a successful decontamination process.
Blunt traumatic injuries often are a result of motor vehicle collisions, explosions, and structural collapses. These various mechanisms can cause fractures, internal hemorrhage, contusions, and internal organ injuries. Recognizing internal hemorrhage and achieving definitive management as fast as possible can be lifesaving. Definitive management for intra-abdominal bleeding and splenic or liver lacerations can involve interventional radiology and/or surgical intervention.
Penetrating traumatic injuries often are secondary to gunshot wounds, stab wounds, and shrapnel from explosions. These can cause internal injuries, including hemorrhage, fractures, and organ perforation. This injury pattern also can cause superficial problems, such as open wounds, that can lead to infection.
Hemorrhagic shock is a common complication of trauma and MCIs. Initial hemorrhage control with tourniquets and hemostatic dressings often occurs on scene. Balanced resuscitation helps to prevent coagulopathy that occurs during trauma. The trauma triad of death is multifactorial and consists of hypothermia, acidosis, and coagulopathy. The coagulopathy aspect involves activation of protein C, platelet dysfunction, and fibrinogen depletion.10,11 Ways to combat the triad of death are administering balanced resuscitation and minimizing crystalloid use. Balanced resuscitation consists of a 1:1:1 ratio of packed red blood cells, plasma, and platelets. When a large volume of resuscitation is needed, a massive transfusion protocol (MTP) can assist in fast and effective delivery of these blood products. Tranexamic acid (TXA) given within three hours of the traumatic injury can reduce bleeding, and, it is hoped, prevent morbidity and mortality. Administration of calcium during large volume transfusion helps reduce hypocalcemia, which, if left untreated, could lead to confusion, muscle spasms, and arrhythmias.12,13
Burns often are secondary to fires, explosions, and chemical spills. They can range from superficial to full thickness and also can affect the airway. Burn injuries often carry high morbidity and mortality.14 Burn resuscitation requires strict fluid resuscitation and treatment at a burn center. Certain lesions may require skin grafting and may require continued care after the initial injury. Burns with airway involvement may require intubation for respiratory support. Initial management should start with airway assessment and vital signs. This then should be followed by the calculation of the extent of burns/total body surface area (TBSA) involved. Based on TBSA, patients should be transported to an appropriate level of care, including burn centers, for fluid resuscitation, debridement, skin grafting, and wound care.
Traumatic brain injuries, head trauma, and spinal injuries are additional possible injuries, especially from blunt trauma. These can range from concussions, contusions, and skull fractures to intracranial hemorrhage and diffuse axonal injuries. Spinal injuries include fractures, dislocations, and even spinal cord injuries. Depending on the severity of the head or spinal injury, some of these patients may require transport to a center with neurosurgical resources.
One paper by Sever et al describes how destructive and non-destructive disasters can lead to various injuries, especially orthopedic and crush injuries.15 (See Table 2.) Crush injuries can be more detrimental than just the initial injury because they can cause rhabdomyolysis and severe metabolic derangements. Early and aggressive fluid resuscitation, allowing for adequate renal perfusion and urinary output, is key in preventing renal injury. If renal injury has occurred, some cases may require renal replacement therapy with hemodialysis. Monitoring electrolytes, especially potassium, is important to prevent life-threatening arrhythmias.
An additional complication of a crush injury is compartment syndrome. Compartment syndrome is diagnosed with both the physical exam and compartment pressures. Patients often have pain out of proportion, paresthesia, pain with passive stretch, and tense compartments. Delta pressure (diastolic blood pressure minus compartment pressure) less than 30 mmHg is strongly suggestive for compartment syndrome. The diagnosis of compartment syndrome is time sensitive, and the treatment is surgical intervention with a fasciotomy.16
Table 2. Complications of Crush Injury |
|
Adapted from: Sever MS, Katı YA, Özkaya U. Destructive disasters, trauma, crush syndrome, and beyond. Acta Orthop Traumatol Turc. 2023;57(6):305-314. |
Depending on the weather, patients also may be exposed to temperatures and environments that put them at risk for hypothermia. The lethal triad of trauma consists of hypothermia, acidosis, and coagulopathy. Hypothermia impairs coagulation by inhibiting enzymatic reactions in the clotting cascade and platelet function.17 This can be managed initially with passive rewarming using blankets, clothing, and insulation to prevent heat loss. Active rewarming more often is performed in a hospital setting with the Bair Hugger, heat packs, and heated blankets. More invasive measures, such as warm intravenous (IV) fluids and intravascular temperature control catheters, also can be used.18
Preparation for Mass Casualty Incidents
Preparation for MCIs is essential, and many different components, including community resources, prehospital resources, and hospital systems, must be included to enhance communication and responses. A common way to prepare for these high-acuity but low-frequency events is through various types of simulation.19 Simulation and tabletop exercises, where a group of people analyze and discuss hypothetical emergency situations, allow for different institutions to formalize procedures, develop appropriate lines of communication, establish leadership, and identify potential areas for improvement. Simulating an MCI can be difficult, but with practice, providers can develop a framework to use in a time of need. As the world develops and technology progresses, the nature of MCIs and the response to them does as well. After an incident, a thorough review of the response is necessary to see what areas need improvement. While no two events are exactly the same, identifying common themes for improvement can be helpful in improving processes for the future.
Knowing patterns of MCIs can help administrators with preparation and protocols. At the same time, these plans also need to be able to accommodate whatever event occurs during any time and in any environment. Flexibility and adaptability are extremely important when caring for MCI victims. It is impossible to prepare for every situation, but frequent exercises, simulation, and review can allow clinicians to be prepared when these events occur.
Strong disaster response systems should include well-established leadership, strong lines of communication, appropriate triage systems, and the ability to establish safety and security. Responding effectively often requires multiple teams, such as local search and rescue, law enforcement, paramedics, and hospitals. Mass casualty preparedness should be an iterative process to improve the tiered and multidisciplinary approach, as noted by Gabbe et al.20 Communication is one of the most important aspects in terms of MCI response. A lack of communication can destroy even the best plans.
Prehospital Response and Triage
An important aspect in prehospital care during an MCI is establishing an incident command center.21 Incident command centers function as the operational centers during an MCI, with the ultimate goal of moving patients to the right place in the most efficient way and allocating resources effectively. Information also can be brought to a central source and can improve both communication and overall assessment of the situation. Communication between the onsite providers and EMS with the expecting hospital is key. Accurate information on the number of patients, distribution of injuries, and resources that will be needed is important to communicate as early as possible.1 In a study reviewing mass casualty terrorist incidents, communication failure commonly was reported, leading to underpreparedness and inefficiency in a time when those are most important.22
Prehospital response and coordination are critical during MCIs. Patients often have time-sensitive injuries. The goal of triage in the prehospital setting is to transport the sickest patients first. Different systems are used to triage patients in the prehospital setting, with the goal of getting people to the most appropriate center within the shortest period. The most widely used triage systems in the United States are Simple Triage And Rapid Treatment (START) and Sort, Assessment, Life-saving interventions, Treatment and Transport (SALT). START is widely used in the United States for adults, and JumpSTART is used for pediatrics.23 The systems use color-coding for patients based on the severity of the illness and timing of treatment needed. Patients tagged with the color black are either deceased or have injuries that are incompatible with life and are not moved to the transfer point. Patients labeled with the color red have severe injuries that could be survivable and should be the first to move to the collection point. Patients designated with the color yellow have serious but not immediate life-threatening injuries and can be transferred at a later time. Patients designated with green are the walking wounded, meaning they can wait to receive medical attention.
Another triage system is SALT, which uses a different technique to categorize patients based on their ability to hear, follow commands, and ambulate on the scene. See Figure 2 for a diagram of SALT triage. SALT triage also uses a color-coded system but has an extra category compared to START. In SALT triage, there are similar designations of green (minimal), yellow (delayed), red (immediate), and black (dead), but the system also includes a gray tag. This gray tag delineates expectant patients, or those patients who are not dead but are not expected to survive with the current situation and resources available. This method then leaves providers with patients who are either unconscious, unable to ambulate, or confused to be attended to first. This system also has providers act on life-threatening injuries during the triage process rather than after the process has been completed.
Figure 2. SALT Mass Casualty Triage |
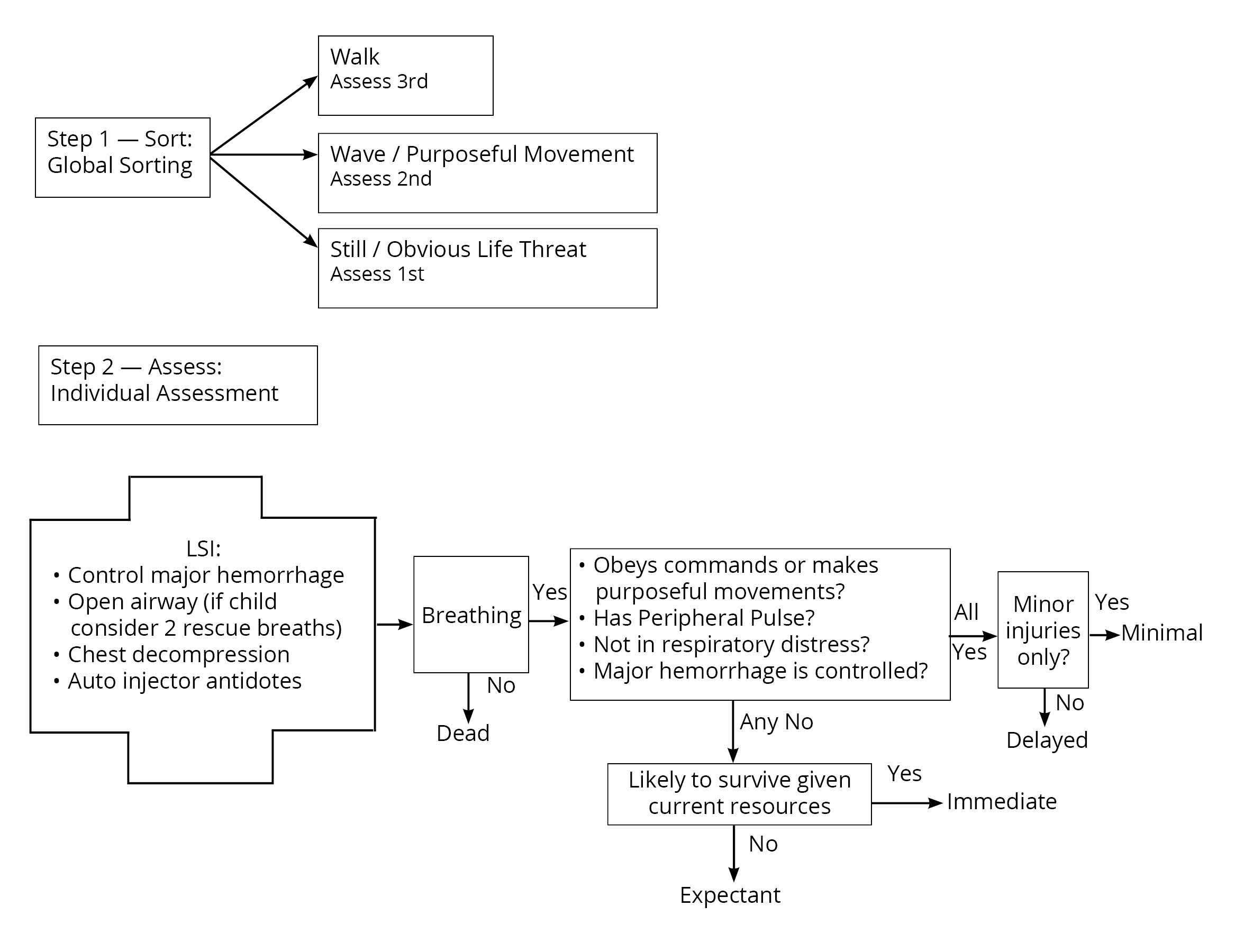 |
Source: Mehralian G, Pazokian M, Akbari Shahrestanaki Y, et al. Development and validation of SALT triage method to facilitate the identification and classification of patients in mass casualty incidents. J Inj Violence Res. 2023;15(2):137-146. Creative Commons 3.0 |
Unfortunately, children often are involved in these incidents, and sometimes approaching these victims from a different perspective can be beneficial. This different approach can start at the triage process. One study looked at a simulation involving JumpSTART and START in triaging patients from an MCI in the setting of pediatric emergency medicine.24 In pediatric MCIs, it has been found that JumpSTART has been faster in triaging patients compared to SALT.25 Some reasons why pediatric patients need a different triage system is because of anatomic and physiologic differences and inability to follow commands reliably. Having adjustments in the triage system attempts to accommodate for these differences. As an example, since pediatric patients more commonly have respiratory failure as an etiology for cardiac arrest, rescue breaths are included in both triage systems; if effective, the patient is triaged as immediate.
Prehospital Interventions
Prehospital care has a critical role in the treatment of MCI patients. Hemorrhage control is extremely important in the setting of severe and life-threatening bleeding. EMS crews have tourniquets and hemostatic dressings that are essential to have on scene. Slowing blood loss can save limbs and lives. Airway management also is a top priority. Initial maneuvers such as head tilt/chin lift and jaw thrust can be performed. If those maneuvers do not work, oropharyngeal or nasopharyngeal airways and even advanced airway management, such as endotracheal intubation, are treatment options. Respiratory support with supplemental oxygen, bag-valve masks, and ventilatory support also can be provided. Circulatory support can be started by obtaining IV or intraosseous (IO) access. Initial resuscitation can be started with IV fluids.
In cases with concern for spinal injury, spine immobilization can be performed. Initial vital signs, including blood pressure, heart rate, respiration, and oxygen saturation, also can be obtained. This provides a starting point to see if the patient’s clinical course is improving or declining. Initial pain management also can be given.26 The interventions performed will vary based on the resources available to the prehospital providers. These all are initial and temporizing measures with the hope of stabilizing patients to get them to the hospital for more definitive management.
The use of blood products in the prehospital setting is a more recent topic of discussion. A multicenter, randomized controlled trial was performed to assess whether giving prehospital packed red blood cells and plasma reduced morbidity and mortality compared to giving 0.9% sodium chloride fluids.27 The researchers found that there was not a significant difference in mortality or lactate clearance between the two groups. Ultimately, both groups had similar adverse effects. EMS agencies are starting to incorporate prehospital transfusions, and continuing research may be beneficial. The Prehospital Blood Transfusion Initiative Coalition focuses on prehospital transfusion practices and availability in the United States.28 The practicality of blood products in the MCI setting is controversial because resources already are scarce in MCIs and blood often is on a national shortage, bringing into question when providing blood (prehospital vs. hospital) can do the most good.
Hospital Response
Once patients arrive at the hospital, another triage process will be needed to better sort patients and stratify resources. Delays in triage often can be a major bottleneck in the system. Hospital policies for MCIs often are in place, but because of the low frequency of these events, they rarely are tested. Another challenge is that every MCI is different based on incident factors as well as hospital factors on any given day. Incident factors include the number of patients, ages of patients, time of day of the incident, weather, and types of injuries. Hospital factors include arrival times of patients, staffing of the hospital, and hospital resources at that given moment.29
Part of the difficulty in predicting preparedness is the variety of MCI causes, which all lead to different injuries and medical needs and need to be treated in their own appropriate way. Injuries can include burns, eye injuries, penetrating trauma, inhalational injuries, toxin exposures, orthopedic injuries, blunt trauma, blast injuries, and others.
Pediatric MCI patients complicate these difficult situations even further. In one study, Desmond reviewed how the anatomic and physiologic differences in pediatric patients affect the triage and treatment processes.30 For triage and treatment, children need specialized equipment, drug doses, and often specialized personnel. During MCIs with limited resources, caring for children can become even more challenging. Children often need assistance, especially in times of injury/illness. When MCIs occur, children frequently have difficulty moving themselves out of a dangerous situation and often rely on additional help. Their anatomy and physiology make them more vulnerable to toxic effects of chemicals, burns, and long-term consequences. Pediatric trauma patients would benefit most from being treated in a pediatric hospital, but there are multiple factors during an MCI (transportation, resources, etc.) that could limit this and affect the care these patients may receive. Understanding the differences in pediatric patients can assist providers in providing the best care for these patients. Desmond et al called for increased awareness, research, and resource development for pediatric care during MCIs.30
To test current systems, simulations and models often are used. A discrete event simulation model was used to evaluate an acute specialty hospital’s current disaster plan in Vienna, Austria.31 Staribacher et al used physicians, nurses, radiology staffing, emergency department beds, ventilators, and operating rooms as the main resources to study for these models. The researchers then ran different scenarios based on arrival time, number of patients, number of staff, and number of computed tomography (CT) machines. They found that the current policy in place could provide three severely injured patients the life-saving care or surgery they needed. This simulation indicated that their current plan would not meet the needs of an MCI with more than three patients with life-threatening injuries. Hospital systems might consider running simulations to see how their current plan could provide for the care needed if an MCI occurred.
Another study surveyed providers who had a role in caring for victims of MCIs, secondary to terrorist attacks, to obtain an idea of the challenges that they faced.32 The survey concluded that some of the biggest challenges faced during this time involved communication, lack of coordination/organization, insufficient staffing, and lack of training. This article also mentioned that providers thought they needed more knowledge about blast injuries. Regardless of the number of patients or critical injuries, without communication, people will not be able to get the care they need. These studies show that communication needs additional training and focus.
Imaging
Radiography and advanced imaging are extremely important and necessary tools during MCIs.33 Radiography can assist in time-sensitive diagnosis and ensure people receive lifesaving treatments. Having a plan in place for the radiology department may be an important part of the MCI plan. CT scans are used routinely in emergency departments, especially during traumas, but their importance sometimes is taken for granted. CT studies often are used to diagnose traumatic injuries that need surgical intervention. Nasir et al studied how radiology departments can best handle these events and get the appropriate results to providers in a timely fashion.33 Factors that affect the ability to obtain imaging studies include the number of CT technicians, the number of working CT scanners, and the number of radiologists reading the imaging. During an MCI, the need for increased staffing may be helpful, but ultimately the number of working CT scanners could result in a bottleneck.
Ultrasound can be a great tool in both prehospital and hospital settings for evaluating injuries secondary to blunt trauma. Advantages of ultrasound include the fact that the EMS and emergency department providers can perform and interpret these studies instantly. When ultrasounds are performed and interpreted by emergency department providers, the overwhelmed radiology department does not have to be involved, which can dramatically decrease the time until the patient can receive care. For example, when a focused assessment with sonography in trauma (FAST) study is performed and found to be positive in the trauma bay, patients can go straight to the operating room for surgical intervention.
Shokoohi et al studied how ultrasound could be used on scene after targeted automobile ramming mass casualty (TARMAC) attacks because of the specific injury patterns that result from that type of incident.34 The researchers endorsed further research but ultimately concluded that ultrasound, when used by experienced providers, can provide fast and accurate information about possible injuries in the prehospital setting and can assist in the triage process. Wydo et al performed a literature review on the use of ultrasound during MCIs.35 The researchers found that the CAVEAT (chest, abdomen, vena cava, and extremities in acute triage) protocol could be useful in evaluating patients for life-threatening injuries. The CAVEAT protocol uses ultrasound to assess pathology beginning with the most life-threatening. Ultrasound is performed first looking at the chest for pneumothorax. Then it is used to examine the abdomen by performing a FAST exam for any sign of hemoperitoneum or hemothorax. Thirdly, a central venous assessment is performed to examine fluid status. Lastly, the extremities are examined at points of tenderness.
Hospital Response and Challenges
MCIs place significant strain on hospitals, as well as their resources, and challenge their capacity. An additional challenge is the rapid influx of patients. Surge capacity refers to the ability of the hospital to manage patients and conditions above their normal capacity. Staffing, emergency department beds, inpatient beds, and intensive care unit beds and supplies often are strained. Having a surge plan in place can assist in making this process easier. Additionally, being able to offload the hospital by using temporary care facilities or other nontraditional spaces can make a significant difference.
Another topic of discussion is the ability of U.S. trauma centers to meet blood requirements during MCIs.36 Blood products are a critical component of treatment and stabilization of MCI victims. This is especially important with the use of an MTP for balanced resuscitation in massive hemorrhage. MTP consists of red blood cells, plasma, and platelets. Through simulations of different events and estimated requirements, Williams et al concluded that Level I trauma centers in the United States do not have enough on-site blood products for MCIs.36 This usually was because of the lack of platelets needed for massive transfusion. Blood products often are in shortage, and an MCI could quickly use all the products available. Another challenge is allocating the available blood products to patients. Continuing to advocate for blood donations is important to help prepare for the worst. Additionally, having major trauma centers with a strategy for stockpiling products before a major event could be helpful in the future.
In a study by Moran et al, researchers conducted and evaluated structured interviews of employees with different backgrounds after an on-site MCI simulation event.37 This was conducted at a Level I trauma center in the Midwestern United States. They ultimately analyzed four different themes: process, supplies and resources, communication, and roles. They were able to get feedback from the staff who would be handling any MCI. Everyone seemed to acknowledge how roles would change during an MCI, but there was less certainty about what that would look like. A common theme was an overall concern about bed availability and staff scarcity. People emphasized the importance of communication, especially from the scene, to prepare for patients and possible safety threats. Ultimately, through simulation, they were able to bring up concerns and develop possible solutions that are common themes throughout all types of MCIs.
Healthcare teams consist of a variety of workers, from social workers to nurses to technicians to physicians. Trying to train all these roles for what an MCI would look like would be a major challenge. A study in Poland during the COVID-19 pandemic assessed the perception of hospital and individual preparedness for an MCI from physicians, nurses, and paramedics.38 The researchers found that more than half of the respondents never had any MCI training and discovered a gap in knowledge, skills, and competency in different healthcare groups that are responsible for handling an MCI.
A mixed methods study was performed with an online survey followed by an interview of providers involved in the Manchester Arena bombing.39 The researchers found that providers who had undergone some emergency preparedness training felt more comfortable when the bombing event occurred, specifically with coordination, roles, and communication. Another group of researchers performed a cross-sectional study of on-call trauma providers in Norway and concluded that a majority of providers were aware of MCI plans, but very few were competent in them.40
Review of Past MCIs
The Boston Trauma Center Chiefs Collaborative performed a review of the response to the Boston Marathon Bombing in 2013 when there were two explosions near the finish line of one of the largest marathons in the world.41 A total of three deaths and more than 260 injuries occurred. Having many first responders at the marathon proved crucial when disaster struck, and on-site care was provided early. Preexisting emergency plans also assisted in communication and coordination.
Kamler et al performed an extensive literature review of MCI articles and triage evaluations during recent MCIs.23 The researchers recognized that MCIs involve an innate chaos that complicates the use of these triage systems during the actual event. During the Boston bombing of 2013, formal triage tags were not routinely used. However, there was a collection point where victims were triaged, and then critical patients were transported within 60 minutes.
After the Paris attacks of 2015 when multiple suicide bombers and armed gunmen conducted coordinated attacks, the importance of hemorrhage control devices was emphasized.23 Hemorrhage control devices consist of hemostatic dressings such as QuiKClot gauze, tourniquets, and topical hemostatic agents, such as WoundStat.
During the Las Vegas shooting in 2017, many patients were transported by private vehicles without a collection point, and as a result, the hospitals did not have communication about how seriously injured patients were or how many patients were coming. Hospitals that were geographically closer to the event were inundated with patients, and patients were not able to be triaged based on resources deemed available. Because of the nature of MCIs, Kamler et al advocate to further simplify the triage process. They additionally focus on the importance of communication during these incidents.23
The Aftermath
The impact of MCIs on first responders and medical personnel can lead to burnout and emotional distress. The high volume and high acuity of patients requiring care can lead to stress that cannot be prepared for. Emergency services must quickly adapt to the demands of a situation far beyond typical operational levels, and the strain on resources can lead to logistical challenges. Hospitals and emergency departments may be overwhelmed, resulting in delays in treatment and difficult decisions regarding who receives care first. In the aftermath, hospitals and healthcare providers may need to implement long-term recovery plans to address both the physical care needs and the emotional toll on staff.
The initial effects after an MCI typically consist of the fatalities and the physical and emotional trauma experienced by survivors, first responders, and healthcare professionals. Individuals may face severe injuries, ranging from physical disabilities to psychological trauma, and often require long-term care, rehabilitation, and counseling. Families are left to cope with grief, the uncertainty of their loved one’s recovery, and, in some cases, the permanent loss of life. Survivors often struggle with a range of emotional and psychological challenges, including post-traumatic stress disorder (PTSD), anxiety, and depression. A systematic review of the effects of MCIs on prehospital and hospital providers was completed to determine the prevalence and risk factors associated with the development of PTSD, anxiety, depression, and substance use.42 PTSD was found to be the most prevalent mental health outcome. Additionally, nurses reported more mental health conditions than physicians did. Multiple personal factors, such as baseline mental health history, and organizational factors also were involved. Understanding risk factors and prevalence can assist with mitigation strategies and support after an MCI occurs.
The impact on the community cannot be understated. People’s normal lives can be torn apart. Additionally, the economic impact of an MCI also can be significant, particularly if it involves key infrastructure or if it disrupts local businesses and services for an extended period. The consequences and aftermath of an MCI are profound and multifaceted, affecting not only the patients and their families but also communities, healthcare systems, and society as a whole. Another study evaluated characteristics and risk factors associated with post-disaster disease outbreaks.43 This study found that regionally, Africa and the Middle East were most common among those with post-disaster disease outbreaks. They grouped 418 individual risk factors into 14 main clusters. (See Figure 3.) Displacement secondary to a disaster was found to be significantly associated with disease outbreaks. Water, sanitation, and hygiene (WASH) was the second most commonly reported risk factor.
Figure 3. Risk Factors for Disease Outbreaks After a Mass Casualty Incident |
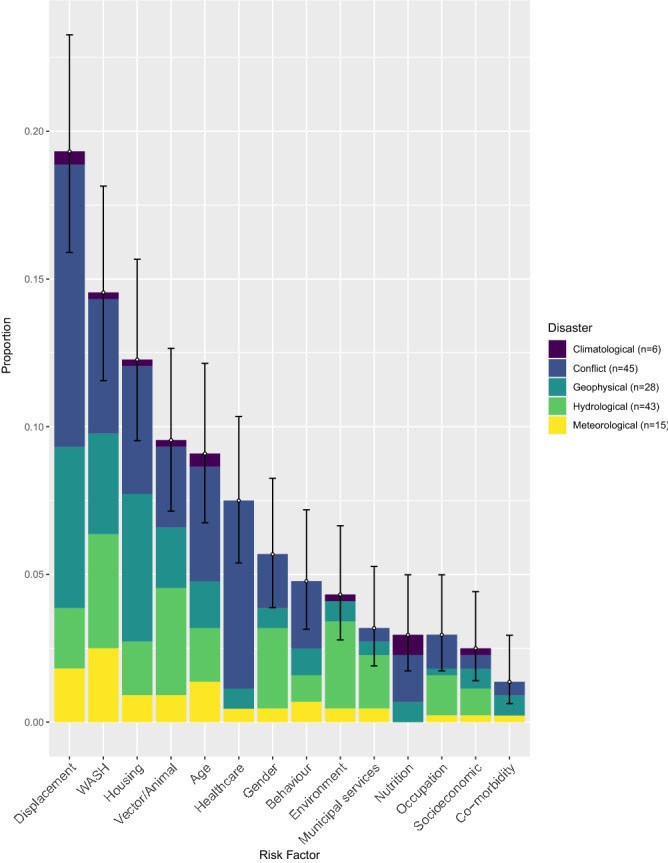 |
Source: Charnley GEC, Kelman I, Gaythorpe KAM, Murray KA. Traits and risk factors of post-disaster infectious disease outbreaks: A systematic review. Sci Rep. 2021;11(1):5616. Creative Commons 4.0 https://creativecommons.org/licenses/by/4.0/ |
To better prepare for future events, addressing the root causes of the incident is important. This can come in the form of policy changes, improved public safety measures, or better preparedness. Analysis can lead to changes in public health protocols, emergency response planning, and safety regulations. Social and governmental responses to MCIs also may spark national or international conversations on issues such as gun violence, disaster preparedness, public health infrastructure, and mental health services. For example, following the terrorist attacks of 9/11, the U.S. government implemented the Public Health and Medical Disaster Response Plan, which coordinated medical teams, hospitals, and psychological services for victims and responders. The World Trade Center Health Program also was created to provide healthcare services to first responders. In response to the mass casualties and overwhelming strain on healthcare systems during the COVID-19 pandemic, many governments provided emergency funding, mental health resources, and mass vaccination campaigns to mitigate the impact on frontline workers and the general public. With all the hardships that come with MCIs, we also can find the goodness and generosity of so many through sacrifice, showing up, and performing heroic tasks for others.
Conclusion
MCIs, ranging from natural disasters to terrorist attacks, are complicated events that involve prehospital and hospital providers. Communication and coordination are important aspects of a successful response to an MCI. Many challenges, such as triaging victims, distributing resources, availability of hospital beds, and timing of lifesaving medical care, exist during an MCI. Having initial plans in place is important, but flexibility during an MCI is key since the situation can change quickly. Learning from previous MCIs helps prepare for the future incidents and ultimately can save lives in the process.
Ellie Ganz, MD, is Chief Resident, The Ohio State University, Columbus. Nicole T. McAllister, DO, MA, is Clinical Assistant Professor of Emergency Medicine, The Ohio State University, Columbus. Whitney Briggs, DO, is Clinical Instructor, University of Arizona.
References
1. DeNolf RL, Kahwaji CI. EMS Mass Casualty Management. In: StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Oct. 10, 2022. https://www.ncbi.nlm.nih.gov/books/NBK482373/
2. Klein TA, Williams J, Irizarry L. EMS Disaster Response. In: StatPearls. StatPearls Publishing; Updated July 17, 2023.
3. Whybark DC. Co-creation of improved quality in disaster response and recovery. Int J Qual Innov. 2015;1:3. https://doi.org/10.1186/s40887-015-0001-y
4. Shackelford SA, Remley MA, Keenan S, et al. Evidence-based principles of time, triage and treatment: Refining the initial medical response to massive casualty incidents. J Trauma Acute Care Surg. 2022;93(2S Suppl 1):S160-S164.
5. Smith A. 2023: A historic year of U.S. billion-dollar weather and climate disasters. Climate.gov. Jan. 8, 2024. https://www.climate.gov/news-features/blogs/beyond-data/2023-historic-year-us-billion-dollar-weather-and-climate-disasters
6. Peterson JK, Densley JA, Hauf M, Moldenhauer J. Epidemiology of mass shootings in the United States. Annu Rev Clin Psychol. 2024;20(1):125-148.
7. Schenk E, Wijetunge G, Clay Mann N, et al. Epidemiology of mass casualty incidents in the United States. Prehosp Emerg Care. 2014;18(3):408-416.
8. Power S, Symons C, Carter H, et al. Mass casualty decontamination in the United States: An online survey of current practice. Health Secur. 2016;14(4):226-236.
9. Collins S, James T, Carter H, et al. Mass casualty decontamination for chemical incidents: Research outcomes and future priorities. Int J Environ Res Public Health. 2021;18(6):3079.
10. Moore EE, Moore HB, Kornblith LZ, et al. Trauma-induced coagulopathy. Nat Rev Dis Primers. 2021;7(1):30. [Published correction appears in Nat Rev Dis Primers. 2022;8(1):25].
11. Buzzard L, Schreiber M. Trauma-induced coagulopathy: What you need to know. J Trauma Acute Care Surg. 2024;96(2):179-185.
12. Van Gent JM, Clements TW, Cotton BA. Resuscitation and care in the trauma bay. Surg Clin North Am. 2024;104(2):279-292.
13. Lier H, Hossfeld B. Massive transfusion in trauma. Curr Opin Anaesthesiol. 2024;37(2):117-124.
14. Hughes A, Almeland SK, Leclerc T, et al. Recommendations for burns care in mass casualty incidents: WHO Emergency Medical Teams Technical Working Group on Burns (WHO TWGB) 2017-2020. Burns. 2021;47(2):349-370.
15. Sever MS, Katı YA, Özkaya U. Destructive disasters, trauma, crush syndrome, and beyond. Acta Orthop Traumatol Turc. 2023;57(6):305-314.
16. Osborn PM, Schmidt AH. Diagnosis and management of acute compartment syndrome. J Am Acad Orthop Surg. 2021;29(5):183-188.
17. van Veelen MJ, Brodmann Maeder M. Hypothermia in trauma. Int J Environ Res Public Health. 2021;18(16):8719.
18. Drumheller BC, Stein DM, Scalea TM. Use of an intravascular temperature control catheter for rewarming of hypothermic trauma patients with ongoing hemorrhagic shock after combined damage control thoracotomy and laparotomy: A case series. Injury. 2018;49(9):1668-1674.
19. Brohi K, Tallach R. Mass casualty medicine: Time for a 21st century refresh. Br J Anaesth. 2022;128(2):e65-e67.
20. Gabbe BJ, Veitch W, Mather A, et al. Review of the requirements for effective mass casualty preparedness for trauma systems. A disaster waiting to happen? Br J Anaesth. 2022;128(2):e158-e167.
21. Lincoln EW, Freeman CL, Strecker-McGraw MK. EMS Incident Command. In: StatPearls [Internet]. StatPearls Publishing; 2024 Jan-. Updated May 16, 2023. https://www.ncbi.nlm.nih.gov/books/NBK534800/
22. De Cauwer H, Barten D, Willems M, et al. Communication failure in the prehospital response to major terrorist attacks: Lessons learned and future directions. Eur J Trauma Emerg Surg. 2023;49(4):1741-1750.
23. Kamler JJ, Taube S, Koch EJ, et al. Effectiveness of and adherence to triage algorithms during prehospital response to mass casualty incidents. J Spec Oper Med. 2023;23(1):59-66.
24. Tan YT, Shin CKJ, Park B, et al. Pediatric emergency medicine didactics and simulation: JumpSTART secondary triage for mass casualty incidents. Cureus. 2023;15(6):e40009.
25. Jones N, White ML, Tofil N, et al. Randomized trial comparing two mass casualty triage systems (JumpSTART versus SALT) in a pediatric simulated mass casualty event. Prehosp Emerg Care. 2014;18(3):417-423.
26. El Sayed M, Tamim H, Mann NC. Description of procedures performed on patients by emergency medical services during mass casualty incidents in the United States. Am J Emerg Med. 2015;33(8):1030-1036.
27. Crombie N, Doughty HA, Bishop JRB, et al. Resuscitation with blood products in patients with trauma-related haemorrhagic shock receiving prehospital care (RePHILL): A multicentre, open-label, randomised, controlled, phase 3 trial. Lancet Haematol. 2022;9(4):e250-e261.
28. Prehospital Blood Transfusion Initiative Coalition. Updated 2024. https://prehospitaltransfusion.org/about/
29. Mohanty CR, Radhakrishnan RV, Stephen S, et al. Epidemiology of mass casualty incidents in a tertiary care trauma center in eastern India: A retrospective observational study. Turk J Emerg Med. 2022;22(2):96-103.
30. Desmond M, Schwengel D, Chilson K, et al. Paediatric patients in mass casualty incidents: A comprehensive review and call to action. Br J Anaesth. 2022;128(2):e109-e119.
31. Staribacher D, Rauner MS, Niessner H. Hospital resource planning for mass casualty incidents: Limitations for coping with multiple injured patients. Healthcare (Basel). 2023;11(20):2713.
32. Tallach R, Einav S, Brohi K, et al. Learning from terrorist mass casualty incidents: A global survey. Br J Anaesth. 2022;128(2):e168-e179.
33. Nasir MU, Chandy PE, Roberts J, O’Neill SB. A guide to mass casualty incidents for radiology residents: Strategies, ethics, directions. Curr Probl Diagn Radiol. 2021;50(5):555-559.
34. Shokoohi H, Pourmand A, Boniface K, et al. The utility of point-of-care ultrasound in targeted automobile ramming mass casualty (TARMAC) attacks. Am J Emerg Med. 2018;36(8):1467-1471.
35. Wydo SM, Seamon MJ, Melanson SW, et al. Portable ultrasound in disaster triage: A focused review. Eur J Trauma Emerg Surg. 2016;42(2):151-159.
36. Williams J, Gustafson M, Bai Y, et al. Limitations of available blood products for massive transfusion during mass casualty events at US Level 1 trauma centers. Shock. 2021;56(1S):62-69.
37. Moran ME, Zimmerman JR, Chapman AD, et al. Staff perspectives of mass casualty incident preparedness. Cureus. 2021;13(6):e15858.
38. Goniewicz K, Goniewicz M, Włoszczak-Szubzda A, et al. The importance of pre-training gap analyses and the identification of competencies and skill requirements of medical personnel for mass casualty incidents and disaster training. BMC Public Health. 2021;21(1):114.
39. Skryabina EA, Betts N, Reedy G, et al. The role of emergency preparedness exercises in the response to a mass casualty terrorist incident: A mixed methods study. Int J Disaster Risk Reduct. 2020;46:101503.
40. Jørgensen JJ, Monrad-Hansen PW, Gaarder C, Næss PA. Disaster preparedness should represent an augmentation of the everyday trauma system, but are we prepared? Trauma Surg Acute Care Open. 2021;6(1):e000760.
41. Boston Trauma Center Chiefs’ Collaborative. Boston Marathon bombings: An after-action review. J Trauma Acute Care Surg. 2014;77(3):501-503.
42. Uddin H, Hasan MK, Castro-Delgado R. Effects of mass casualty incidents on anxiety, depression and PTSD among doctors and nurses: A systematic review protocol. BMJ Open. 2023;13(9):e075478.
43. Charnley GEC, Kelman I, Gaythorpe KAM, Murray KA. Traits and risk factors of post-disaster infectious disease outbreaks: A systematic review. Sci Rep. 2021;11(1):5616.