
Managing Pediatric Wounds
April 1, 2025
Executive Summary
- Several factors can increase the risk of wound infection, including immune-compromising conditions, such as diabetes, asplenism, and immunodeficiency, as well as treatments, such as chemotherapy or corticosteroids.
- Animal bite factors, such as the bite’s location, the nature of the injury, and the type of animal involved are crucial in assessing the risk of infection. High-risk areas include bites to the hands, feet, fingers, genitals, and face, as well as bites that penetrate bones, tendon sheaths, or joint capsules. Dog bites carry a 5% to 25% risk of infection, while cat bites have an infection risk of up to 50%.
- Local anesthesia can be achieved by injecting an anesthetic directly into the wound. To minimize injection pain, the solution should be warmed to 37°C to 39°C, then injected slowly into the subcutaneous tissue (not the dermis) and within open wounds (not intact skin). Using small needles (27 gauge to 30 gauge), limiting needle punctures, and applying a topical anesthetic beforehand can further reduce discomfort.
- Skin adhesives are ideal for small (< 4 cm long), clean, linear, superficial (< 8 mm deep), and well-approximated lacerations.
- The hair apposition technique (HAT) is an effective method for closing simple scalp lacerations using skin adhesives, especially when a patient’s hair is long enough to be twisted. To perform HAT, strands of hair on either side of the laceration are used to approximate the wound edges. The hair strands are twisted together to close the wound, and then a small amount of skin adhesive is applied to the twisted hair.
- Prophylactic antibiotics are advised for high-risk animal bites. Amoxicillin-clavulanate is commonly prescribed for three to five days, since it covers pathogens such as Pasteurella multocida, Capnocytophaga canimorsus, Staphylococcus species, Streptococcus species, and anaerobes.
Wounds are a common and critical aspect of emergency medicine practice. Children pose unique challenges, which are comprehensively reviewed by the authors with strategies for optimal management.
— Ann M. Dietrich, MD, FAAP, FACEP, Editor
By Mia Karamatsu, MD; Brittany Boswell, MD; and Cherelle Smith, MD, MS
Introduction
A wound is an injury that is defined as damage to a membrane (e.g., skin or mucosal surface), such as a laceration, bite, abrasion, or puncture. When considering pediatric patients, wound types and locations often are dependent on the child’s age and development. Proper wound care is important to prevent infection and minimize scarring. Additionally, a patient’s vaccination status should be considered to determine the risk of tetanus infection in all patients with dirty wounds. In addition, they may require surgical subspecialty consultation, depending on the extent of the injury. This review will focus on the management of lacerations, animal bites, and common types of acute pediatric wounds that require medical intervention.
Etiology and Epidemiology
In the United States, approximately 12 million skin wounds are treated in emergency departments (EDs) annually.1 In 2002, lacerations in children (ages 0-17 years) accounted for 8.2% to 8.6% of ED visits.2 Compared to adults, children’s lacerations more frequently were located on the head, shorter in length, less contaminated, and more commonly resulted from blunt trauma.1,3
Animal bites are a common occurrence worldwide. In the United States, dog bites account for 85% to 90% of all animal bites, followed by cats at approximately 5% to 10%.4,5 Children make up the majority of dog bite victims, with bites most commonly affecting the head and neck in patients younger than 10 years of age.6 From 2001-2017, an estimated 2.4 million children (0-19 years) were treated in U.S. EDs for non-fatal dog bites.7 In 2017, the rate of dog bite ED encounters was 22.3 per 10,000 children (age < 18 years).8
Etiology/Pathophysiology
There are four overlapping stages of wound healing: hemostasis, inflammation, proliferation, and maturation/remodeling. If any of these stages are disrupted, it can lead to abnormal healing and scarring. The process of wound healing takes months and can last for up to two years.9 The key factors for effective healing are wound hydration, adequate perfusion, minimizing trauma, and infection control.10
Evaluating the Wound
Obtaining a thorough history is important to assess risk factors for infection, associated injuries, and the ability of the patient to heal properly. Asking about the mechanism of injury is critical. For example, if a toe laceration is caused by a crush injury, there may be an underlying fracture. Or, if the finger wound is caused by a cat bite, it is considered at high risk for an infection. When performing a physical exam, the size and depth of the wound(s) should be documented. The wound edges also need to be examined, since that will help determine the closure method. After a focused history and exam, the need for imaging should be determined. Plain radiographs can help detect fractures in crush injuries and identify retained foreign bodies. Advancements in artificial intelligence (AI) digital imaging technology have the potential to transform wound assessment in pediatric emergency care. Zoppo et al reported on an AI-powered portable medical device that can evaluate and classify ulcerated wounds with 97% accuracy.11 This technology enhances measurement standardization and documentation consistency.
Risk for Infection
Several factors can increase the risk of wound infection, including immune-compromising conditions, such as diabetes, asplenism, and immunodeficiency, as well as treatments, such as chemotherapy or corticosteroids. Assessing tetanus vaccination status is crucial, especially for contaminated wounds. Additionally, the type, contamination level, and depth of the wound play key roles in infection risk.
The traditional belief in a strict “golden period” for wound closure is not well-supported by high-quality evidence.12 Instead, studies highlight specific risk factors for infection. One study found that all initially infected wounds were older than 18 hours, with a 1.2% infection rate after repair.13 Risk factors included prophylactic antibiotic use, subcutaneous sutures, wounds > 5 cm, glass or ice injuries, and extremity location.13 Another study identified diabetes, wound length > 5 cm, lower extremity location, and moderate to heavy contamination as independent infection risk factors.14
Contaminated wounds not only carry a risk of infection but also may contain spores that cause tetanus. Wounds exposed to dirt, feces, soil, or saliva (e.g., animal bites) have a higher risk and require thorough irrigation and debridement.15 To prevent tetanus, it is essential to assess the patient’s vaccination status. The U.S. Centers for Disease Control and Prevention (CDC) immunization schedule recommends a five-dose diphtheria, tetanus, and pertussis series for children at 2, 4, 6, and 15-18 months of age, with a final dose at 4-6 years of age, and a tetanus, diphtheria, and pertussis booster for adolescents at 11-12 years of age.16 A study found that emergency physicians incorrectly assessed tetanus prophylaxis in nearly 9% of cases, while another study showed that 25% of 743 children received the tetanus vaccine unnecessarily.17,18 These findings highlight the importance of reviewing a patient’s vaccination history and following CDC guidelines for tetanus prevention. A table summarizing tetanus prophylaxis can be found at https://bit.ly/3DZjrWO.
Animal bites carry a high risk of infection because of their gross contamination. Factors such as the bite’s location, the nature of the injury, and the type of animal involved are crucial in assessing the risk of infection. High-risk areas include bites to the hands, feet, fingers, genitals, and face, as well as bites that penetrate bones, tendon sheaths, or joint capsules.20,21 Dog bites carry a 5% to 25% risk of infection, while cat bites have an infection risk of up to 50%.21,22 Cat bites have a higher predilection to infection because of the deep and puncture-type wounds. Infections from dog and cat bites typically are caused by a mix of aerobic and anaerobic bacteria, with two to five different pathogens often present.21 Common bacteria include Pasteurella species (e.g., Pasteurella multocida), Staphylococcus, Streptococcus, anaerobes like Fusobacterium, Prevotella, Bacteroides, and Porphyromonas. P. multocida usually causes infection within hours, presenting with significant pain and inflammation. Capnocytophaga canimorsus, an emerging pathogen, can lead to systemic infections, such as sepsis.21
In the Untied States, the incidence of rabies in humans is extremely low. Between 1960 and 2018, 125 human rabies cases were reported in the United States. Of these, 89 were acquired in the United States, with 62 (70%) linked to bats, while 36 resulted from dog bites during international travel.23 The primary reservoir species responsible for spreading rabies in the United States are bats, raccoons, skunks, foxes, and mongooses, but any wild or domesticated animals can be carriers for the rabies virus.24
When assessing rabies risk, emergency providers should determine if the bite was provoked or unprovoked, if the animal is vaccinated, and if it is available for observation. Bat bites, which may not leave noticeable marks due to small teeth, should be tested for rabies if possible. If the bat is rabies-free, post-exposure prophylaxis (PEP) is not needed. (See Table 1.) However, if the bat is unavailable for testing or if exposure (e.g., bite, scratch, or mucous membrane contact) cannot be ruled out, PEP is recommended, especially in cases involving vulnerable individuals, such as children or intoxicated persons.25,26
Table 1. Post-Exposure Prophylaxis (PEP)27 |
||
| Patient Population | Treatment Options | Post-Exposure Recommendations |
All patients |
Wound cleansing |
All PEP should begin with immediate thorough cleansing of all wounds with soap and water. If available, a virucidal agent, such as a povidone-iodine solution, should be used to irrigate the wounds. |
Non-immunized patients |
Human rabies immune globulin |
If possible, the full dose should be infiltrated around any wound(s) and any remaining volume should be administered intramuscularly at an anatomical site distant from vaccine administration. Also, human rabies immune globulin should not be administered in the same syringe as a vaccine. Because human rabies immune globulin might partially suppress the active production of antibodies, no more than the recommended dose should be given. |
Vaccine |
Human diploid cell culture rabies vaccine or purified chick embryo cell vaccine 1.0 mL, intramuscularly in the deltoid area (for children anterolateral aspect of the thigh is acceptable), one each on days 0, 3, 7, and 14. A fifth dose on day 28 is recommended for persons with a confirmed or suspected immune disorder. Vaccines should never be administered in the gluteal area. |
|
Previously immunized patients |
Human rabies immune globulin |
Rabies immune globulin should NOT be administered. |
Vaccine |
Human diploid cell culture rabies vaccine or purified chick embryo cell vaccine 1.0 mL, intramuscularly in the deltoid area (for children anterolateral aspect of the thigh is acceptable), one each on days 0 and 3. Vaccines should never be administered in the gluteal area. |
|
Wound Treatment/Management
If the wound resulted from significant trauma, the patient should undergo primary and secondary surveys according to Advanced Trauma Life Support guidelines. During these surveys, the wounds are identified and assessed. The initial step is to achieve hemostasis, and for wounds with vascular injury, a pressure bandage or tourniquet may be required. Once the patient is stable, pain should be evaluated and treated. The next steps in treatment will depend on the location, size, depth, and nature of the wound.
Analgesia and Anesthesia
The patient may receive an oral, intranasal, intravenous, or intramuscular analgesic based on the severity of the wound and pain level. Providing adequate analgesia is crucial for proper wound care, since insufficient pain relief can lead to more procedure complications, heightened sensitivity to pain in the future, and increased anxiety about medical care.28
Oral analgesics, such as acetaminophen and ibuprofen, commonly are given to children while waiting for topical anesthetics to take effect. Pediatric patients generally do not require opioids for pain relief, although they may be needed for those with significant injuries, such as fractures or dislocations. Opioids can be administered orally, intranasally, intravenously, or intramuscularly. If used, patients must be closely monitored for potential side effects (e.g., respiratory depression, nausea, vomiting).
In preparation for wound repair, a topical anesthetic, such as lidocaine (4%), epinephrine (0.1%), and tetracaine (0.5%) gel (LET) should be applied 20 minutes to 30 minutes prior to the procedure for optimal effect, especially in highly vascularized areas, such as the face and scalp.29 Other options no longer include an eutectic mixture of local anesthetics; lidocaine, prilocaine (EMLA); and tetracaine, adrenaline, and cocaine (TAC) because EMLA is Food and Drug Administration-approved only for intact skin because of the risks of toxicity on open wounds, and TAC is no longer used because of the risks of toxicity. For mucosal surfaces, viscous lidocaine and benzocaine are used, but viscous lidocaine carries a black box warning for children younger than 3 years of age because of the risks of seizures, cardiopulmonary arrest, and death from improper use. Additionally, methemoglobinemia can occur with topical lidocaine and benzocaine, especially in patients younger than 2 years of age.30
Local anesthesia can be achieved by directly injecting an anesthetic into the wound. To minimize injection pain, the solution should be warmed to 37°C to 39°C, then injected slowly into the subcutaneous tissue (not the dermis) and within open wounds (not intact skin). Using small needles (27 gauge to 30 gauge), limiting needle punctures, and applying a topical anesthetic beforehand can further reduce discomfort.31,32 Lidocaine has a fast onset (< 1 minute) with a shorter duration of effect when compared to bupivacaine. The addition of epinephrine can prolong the anesthetic effect, delay systemic absorption, and help control local bleeding.32
Regional or digital nerve blocks are an excellent alternative to local infiltration for larger lacerations or injuries to the digits. They offer effective pain relief without distorting the wound margins. Historically, epinephrine was avoided in digital blocks because of concerns about ischemia and necrosis. However, evidence has shown that, in healthy patients, it is both safe and beneficial.32,33 Table 2 summarizes anesthetic options for local, regional, and digital anesthesia.
Sedation or anxiolysis may be required for wound repair in children, especially for complex repairs or wounds in cosmetically sensitive areas. When administered properly, medications such as ketamine, midazolam, nitrous oxide, and dexmedetomidine are both effective and safe.34 Ketamine, which acts as both a sedative and analgesic, can be given via intranasal (IN), intramuscular (IM), or intravenous (IV) routes, although it rarely is administered orally because of its wide therapeutic window.35
Table 2. Anesthetic Options for Local, Regional, and Digital Anesthesia30,32 | |||
| Anesthetic | Duration of Effect | Adult Maximum Dose | Pediatric Maximum Dose |
Lidocaine | 30 minutes to 45 minutes | 300 mg | 1.5 to 2.0 mg/kg |
Bupivacaine | 120 minutes to 240 minutes | 175 mg | 2.0 mg/kg |
Lidocaine with epinephrine | 60 minutes to 400 minutes | 500 mg | 3.0 mg/kg to 4.5 mg/kg |
Bupivacaine with epinephrine | 240 minutes to 480 minutes | 225 mg | 3.0 mg/kg |
For cases requiring only anxiolysis, midazolam and inhaled nitrous oxide are well-tolerated options. Midazolam typically is given orally or IN, while nitrous oxide typically is delivered as a 50% nitrous oxide/50% oxygen mixture. Dexmedetomidine provides sedative, anxiolytic, and analgesic effects but carries a higher risk of bradycardia and hypotension. Notably, it has been successfully used for sedation in children with autism spectrum disorder.36 Another important factor to consider is the calming presence of a parent, which can help decrease the need for analgesia, sedation, and/or anxiolysis.37 Pharmacological interventions should be customized to meet the specific needs of each patient.
Child life specialists play a crucial role in the ED by addressing the psychosocial needs of pediatric patients and their families. They prepare the patient for the procedure using developmentally appropriate communication and play.38
If a child life specialist is unavailable, technology can be used to distract pediatric patients during procedures. Options like watching movies, playing video games, or using immersive virtual reality (VR) goggles can help. For example, watching cartoons was found to be effective in distracting 3- to 6-year-olds during facial laceration repair.39 A study by McEnvoy et al found that immersive VR goggles significantly reduced pain and fear scores in patients aged 6-17 years during laceration repair while also decreasing anxiolytic use in 12- to 17-year-olds.40
When adapting wound care for children with special healthcare needs, research shows that thoughtful modifications can significantly improve outcomes. Thompson and Tielsch-Goddard’s research highlights how tailored preparation approaches for children with autism spectrum disorder can transform procedural experiences in medical settings.41 Their findings suggest that personalized visual aids and environmental adaptations designed to address sensory sensitivities substantially reduce disruptive behaviors during procedures. The researchers observed that families reported markedly better experiences and decreased anxiety levels when these specialized techniques were implemented during medical interventions, including wound care procedures. These evidence-based strategies offer practical solutions for emergency providers managing wounds in children with developmental differences.41 Their research highlighted that allowing additional time for procedures and using preferred sensory items enhanced compliance and outcomes for these children.
Irrigation
All wounds with potential contamination should be carefully and thoroughly cleaned. Multiple studies indicate that the choice of irrigation solution (e.g., tap water, saline, sterile water) does not affect the risk of infection.42,43 Leading surgical and trauma organizations emphasize the importance of proper source control through cleaning, irrigation, and disinfection for all skin and soft tissue injuries, including mammalian bites.44
Debridement
Torn, crushed, and devitalized tissue will require debridement. This will help to promote proper healing once the wound is closed. Joint involvement will require subspecialty consultation for surgical debridement.
Gloves
Studies have demonstrated that there is no clinically important difference in infection rates between using clean non-sterile gloves and sterile gloves during the repair of traumatic lacerations in the ED.45,46 Based on the evidence, clean non-sterile gloves provide a safe, effective, and cost-efficient alternative to sterile gloves for laceration repair in the emergency department.
Wound Closure
There are three methods for wound closure: primary closure, secondary intention, and delayed closure. Primary closure involves fully approximating the wound edges using sutures, staples, or tissue adhesive. Secondary intention allows the wound to heal naturally without closure, while delayed closure is used when infection risk is high, with final repair done later.
Healing time depends on wound depth and location, with well-vascularized areas, such as the face and head, healing more quickly, while the extremities and digits take longer. In the ED, primary closure is commonly used for acute wounds. However, high-risk animal bites may be left to heal by secondary intention to reduce infection risk. The choice of repair method depends on multiple factors, such as wound type, size, depth, location, and tension.
Staples
Staples are quick and easy to apply, requiring minimal training, and are effective for rapidly controlling scalp or extremity hemorrhages, particularly in mass casualty situations. They are cost-effective, simple to remove, and offer infection rates and healing times comparable to sutures. This makes them an excellent choice for treating large scalp lacerations in children.
Skin Adhesive and Adhesive Strips
Skin adhesives, like Dermabond, have been widely used for laceration repair since their introduction more than 20 years ago. These adhesives consist of liquid cyanoacrylate monomers that polymerize into solid chains upon contact with tissue, drying within minutes. They are ideal for small (< 4 cm long), clean, linear, superficial (< 8 mm deep), and well-approximated lacerations.47 This method offers a faster, less painful alternative to sutures and has similar cosmetic outcomes.2,48
Patients with wounds repaired with skin adhesives have shorter ED stays compared to those with sutures or staples.49 For optimal results, the wound should be hemostatic, clean, dry, and well-aligned before application, and a topical anesthetic, such as LET, can help achieve hemostasis and alleviate discomfort during the adhesive’s application.
The hair apposition technique (HAT) is an effective method for closing simple scalp lacerations using skin adhesives, especially when a patient’s hair is long enough to be twisted. To perform HAT, strands of hair on either side of the laceration are used to approximate the wound edges. The hair strands are twisted together to close the wound, and then a small amount of skin adhesive is applied to the twisted hair. Visual aids of the HAT can be found at https://bit.ly/4kKkQRA. This process is repeated until the entire laceration is closed. It is a well-tolerated technique, particularly in children.50
Skin adhesives are not recommended for stellate lacerations, puncture wounds, bites, or heavily contaminated or infected wounds. They also are not ideal closure methods for wounds under significant tension or on areas with high mobility (e.g., joints, mouth).
Adhesive strips, such as Steri-Strips, can be used alone or alongside a skin adhesive to close small, linear lacerations that do not require multilayer closure. A randomized controlled trial by Munns et al compared skin adhesive alone to skin adhesive with adhesive strips, finding no significant difference in complication rates or cosmetic outcomes.51 Adhesive strips can help align the wound edges before applying the skin adhesive and reduce tension on the wound. Applying a benzoin tincture around the laceration can improve the adhesion of the strips. Patients and families are advised to allow the adhesives to peel off on their own, which typically takes seven to 10 days.
Sutures
There are various types of sutures, including natural, synthetic, absorbable, non-absorbable, multifilament (braided, multiple strands), and monofilament (single strand). Synthetic sutures are preferred for facial wounds because of their minimal reactivity and reduced inflammation. Absorbable sutures typically are used in areas requiring less support and for internal layers. Non-absorbable sutures are chosen when long-term mechanical support is needed. Monofilament sutures are less prone to infection but can be damaged by surgical instruments, while multifilament sutures can harbor infections and are more prone to tangling.
Table 3 summarizes various suture materials for consideration. Table 4 contains recommendations for suture materials based on laceration location and depth.
Table 3. Suture Materials52 | ||||
| Brand Name | Suture Material | Effective Tensile Strength Duration | Tissue Reactivity | Typical Use |
| Absorbable | ||||
Vicryl | Polygalactin 910 | 21 days | Moderate | Deep tissue (dermis, muscle, fascia, oral mucosa, genital) |
Vicryl Plus | Polygalactin 910 treated with antimicrobial | 21 days | Moderate | Deep tissue (dermis, muscle, fascia, oral mucosa, genital) |
Vicryl Rapide | Polygalactin 910 gamma irradiated to speed absorption | Five days | Moderate | Skin |
Monocryl | Poliglecaprone 25 | Seven to 14 days | Minimal | Skin |
Plain Gut | Beef serosa or sheep submucosa | Seven to 10 days | High | Soft tissue |
Fast Absorbing Gut | Beef serosa or sheep submucosa heat treated to speed absorption | Seven days | High | Skin |
Chromic Gut | Beef serosa or sheep submucosa treated with chromium to slow absorption and tissue reaction | 21 days to 28 days | High | Mucosa |
| Non-Absorbable | ||||
Ethilon | Nylon | Gradual loss over time | Minimal | Skin |
Prolene | Polypropylene | Infinite | Minimal | Skin, tendon, ligaments |
Perma-Hand Silk | Silk | Gradual loss over time | High | Temporary hemostasis, bolsters |
Table 4. Recommended Suture Material Based on Laceration Location and Depth | |||
| Location | Wound Character and Depth | Material | Removal Time |
Scalp | Superficial or deep | Hair apposition technique | N/A |
Staple | Seven days | ||
5-0 Ethilon or Prolene | Seven days | ||
Face | Superficial, linear, low-tension | Skin adhesive ± adhesive strips | N/A |
6-0 Monocryl or fast-absorbing gut | N/A | ||
6-0 Ethilon or Prolene | Five to seven days | ||
Deep, high-tension, irregular | 6-0 Monocryl or fast-absorbing gut | N/A | |
6-0 Ethilon or Prolene | Five to seven days | ||
5-0 Vicryl (deep layer) | N/A | ||
Trunk | Superficial, low-tension | 5-0 Vicryl Rapide | N/A |
5-0 Ethilon or Prolene | 10 days | ||
Deep, high-tension | 4-0 Ethilon or Prolene | 10 days | |
4-0 Vicryl (deep layer) | N/A | ||
Extremity NOT involving a joint | Superficial, low-tension | 4-0 or 5-0 Vicryl Rapide | N/A |
5-0 Ethilon or Prolene | 10 days | ||
Deep, high-tension | 4-0 Ethilon or Prolene | 10-14 days | |
4-0 Vicryl (deep layer) | N/A | ||
Extremity involving a joint | Superficial, low-tension | 5-0 Ethilon or Prolene | 10-14 days |
Superficial, high-tension | 4-0 Ethilon or Prolene | 10-14 days | |
Nail bed | Simple or complex | Skin adhesive 6-0 Monocryl or fast-absorbing gut | N/A |
Common suturing techniques include:
- Simple interrupted sutures are a good option for low-tension wounds.
- Mattress sutures (horizontal, vertical) are good for high-tension wounds.
- Half-buried horizontal mattress sutures (also known as a “corner stitch”) are good for V-shaped, Y-shaped, or T-shaped wound edges.
- A two-layer closure method is recommended for deep lacerations where a buried suture closes the deeper layer, followed by sutures closing the skin layer.
Various suture techniques are demonstrated in Figure 1.
Figure 1. Suture Techniques |
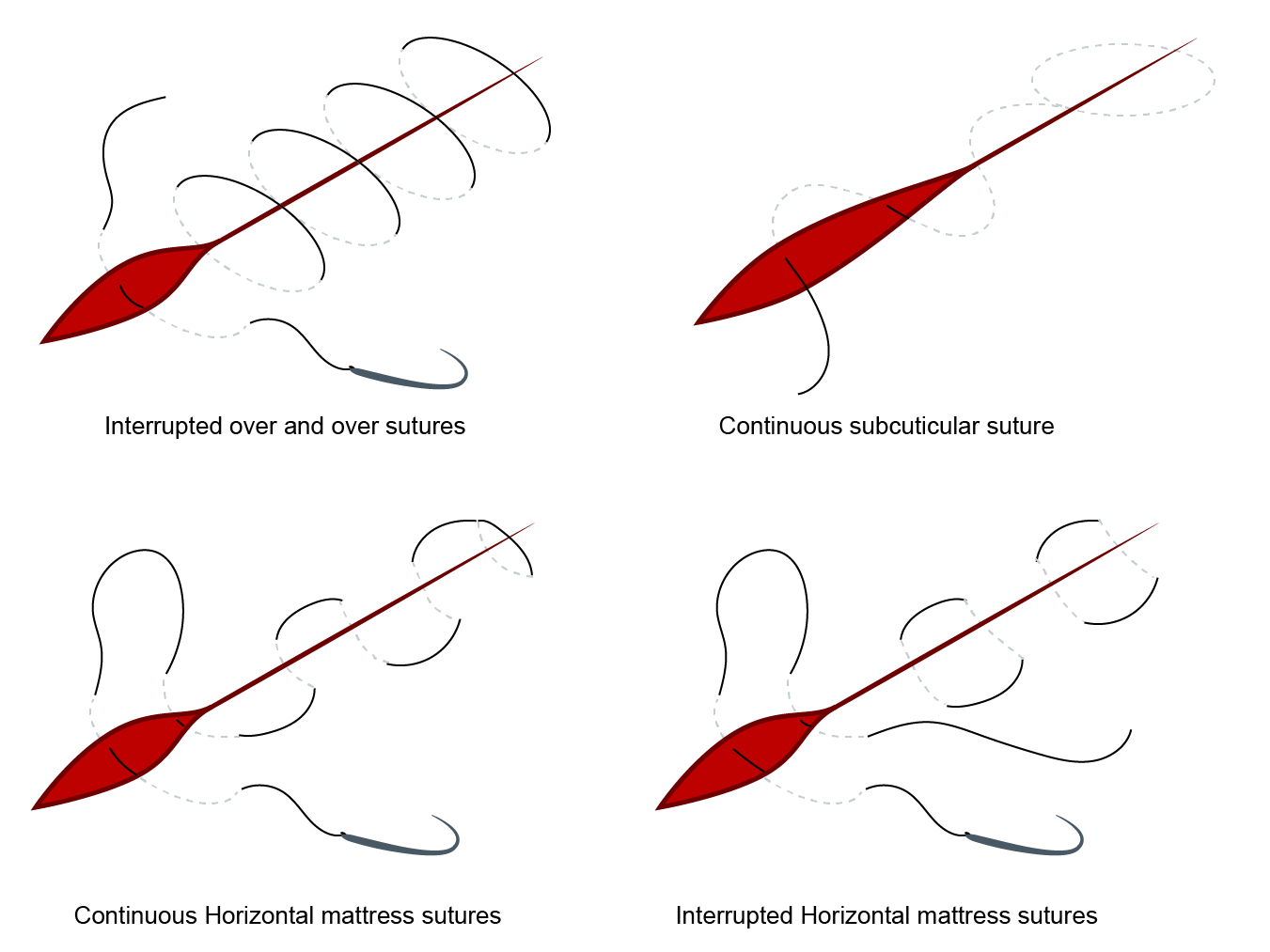 |
Source: Relias |
Nail bed injuries are common in children. Fifteen percent to 24% of children who present with fingertip injuries have a concurrent nail bed laceration.53 Traditionally, nail beds have been repaired with 6-0 absorbable sutures. However, nail bed lacerations can be repaired with tissue adhesive and have similar outcomes as those that were sutured.53
Dermal avulsion can either be partial or complete. For partial avulsions, the affected tissue can be cleaned and used to close the wound gap. However, for completely avulsed tissue, wound closure depends on the extent of tissue loss. In cases where the dermal avulsion involves the pulp of the fingertip, there are two management approaches. The first steps are to control pain and achieve hemostasis. Begin by performing a digital block and having the patient soak the fingertip in 1% lidocaine with epinephrine for 10 minutes. Next, apply a tourniquet to the affected finger and dry the wound. The first option is to apply tissue adhesive to the hemostatic wound and ensure the adhesive is completely dry before removing the tourniquet.54
The second option is to apply a hemostatic gauze or gel (e.g., Surgicel or Gelfoam) and hold moderate pressure, then remove the tourniquet. Remove pressure once hemostasis is achieved. Instruct the patient to keep the dressing on as the product liquefies over the next two to five days.55
Antibiotics
Universal prophylaxis is not recommended. Clean, superficial lacerations that have been irrigated and closed with tissue adhesive do not require antibiotics. However, prophylactic antibiotics are advised for high-risk animal bites.
Amoxicillin-clavulanate is commonly prescribed for three to five days, since it covers pathogens such as P. multocida, Capnocytophaga canimorsus, Staphylococcus species, Streptococcus species, and anaerobes. For patients allergic to penicillin, trimethoprim-sulfamethoxazole combined with clindamycin is recommended.
Additionally, patients with lacerations associated with open fractures should receive antibiotic prophylaxis, such as cephalexin, to prevent osteomyelitis.
Scar Minimization
Scar formation can significantly affect a patient’s quality of life physically, socially, and psychologically. To minimize scarring, wound repairs should focus on relieving tension, preventing infection, reducing inflammation, and ensuring proper blood flow to the healing tissue.9 While some children may be prone to hypertrophic scars or keloids, most can heal well with proper nutrition and wound care. For deep wounds, a two-layer closure and adhesive strips can help reduce tension. Studies suggest that applying adhesive tape (e.g., Steri-Strips) immediately postoperatively and for long-term management can decrease scarring.56 Silicone gel sheeting also may help, although evidence is mixed.57,58 Contaminated wounds require proper wound irrigation and antibiotic prophylaxis to prevent infection. Topical antibiotic ointments or petroleum-based ointments can help keep the wound moist and promote healing.44,59
Keeping the wound moist accelerates epithelialization and healing.10 While antioxidants, such as vitamins C and E, are thought to aid healing, there is insufficient evidence to confirm their effectiveness.9
Cosmetic Outcomes
A systematic review and meta-analysis by Tandon et al found that tissue adhesive, adhesive tape, and sutures had equivalent risks of wound infection and dehiscence in pediatric patients undergoing primary wound closure, with adhesive tape showing slightly better cosmetic outcomes.60 Similarly, a small study by Barton et al on simple pediatric lacerations (≤ 5 cm long, ≤ 0.5 cm wide, < 12 hours old) found no significant difference in cosmetic outcomes between absorbable sutures, Dermabond, and Steri-Strips after three months.61
Special Considerations
Most pediatric lacerations do not require consultation with specialists, such as plastic surgery, otolaryngology, oral-maxillofacial surgery, or ophthalmology. A study by Miller et al found that the median consultation rate for facial lacerations in pediatric EDs across the United States and Canada was 10%, consistent with previous studies reporting rates of 7% and 14%.13,62,63 Some institutions had specific criteria for consultation, including involvement of the medial canthus, tarsal plate, facial cartilage, oral commissure, ala, deeper structures (bones, muscles, blood vessels, nerves), or tissue loss. When subspecialists repair these complex lacerations in the ED, sedation often is required, significantly increasing the patient’s length of stay.62
Cultural competence represents an essential element in providing effective pediatric wound care. Research has demonstrated that culturally sensitive approaches directly affect treatment outcomes across diverse patient populations.64 Brotanek and colleagues emphasize that understanding a family’s cultural framework significantly influences their perception of treatments and adherence to wound care instructions.65 When healthcare providers incorporate culturally informed approaches, they create opportunities for improved communication regarding wound healing expectations and home care practices. The American Academy of Pediatrics (AAP) reinforces this principle, noting that culturally effective care requires providers to recognize how cultural beliefs may shape families’ responses to medical interventions, including wound management strategies.66 Implementing these culturally responsive techniques in emergency settings can lead to measurable improvements in patient satisfaction, treatment adherence, and clinical outcome. Cultural competence is an important consideration and should be applied to pediatric wound care as well.
Prognosis and Follow-Up
After discharge from the ED, some patients may need to follow up with their primary care provider for a wound check and, if necessary, suture or staple removal. Before discharge, patients and their families should receive instructions on proper wound care, pain control, scar minimization techniques, and antibiotic use (if prescribed). It is essential to review return precautions, including signs of infection or wound dehiscence.
Summary
Proper management of pediatric lacerations and animal bites is essential to prevent infection, promote healing, and reduce scarring. Initial evaluation involves assessing wound depth, contamination, and the risk of complications such as rabies or tetanus. Addressing the child’s pain and providing medication for anxiety or sedation, when necessary, can improve the treatment experience. Collaborating with child life specialists (if available) and using distraction techniques helps create a psychologically supportive environment. Thorough irrigation is critical for cleaning contaminated wounds. Closure techniques depend on factors like location, size, depth, and infection risk. Smaller, simple lacerations may be closed with skin adhesives (e.g., glue, tape), while larger, more complex wounds often require sutures. In cases of high infection risk, delayed closure may be necessary. Antibiotic prophylaxis is recommended for certain animal bites, especially deep wounds or those inflicted by cats. Rabies PEP should be considered based on the type of animal, circumstances of the bite, and the animal’s vaccination status. Patient education on wound care and proper follow-up are vital for ensuring optimal healing and preventing complications.
Mia L. Karamatsu, MD, is Assistant Professor of Emergency Medicine and Pediatrics, Stanford University School of Medicine, Stanford, CA.
Brittany Boswell, MD, is Assistant Professor of Emergency Medicine and Pediatrics, Stanford University, Stanford, CA.
Cherrelle Smith, MD, MS, Assistant Professor of Emergency Medicine and Pediatrics, Stanford University, Stanford, CA.
References
- Singer AJ, Dagum AB. Current management of acute cutaneous wounds. N Engl J Med. 2008;359(10):1037-1046.
- Singer AJ, Thode HC Jr, Hollander JE. National trends in ED lacerations between 1992 and 2002. Am J Emerg Med. 2006;24(2):183-188.
- Hollander JE, Singer AJ, Valentine S. Comparison of wound care practices in pediatric and adult lacerations repaired in the emergency department. Pediatr Emerg Care. 1998;14(1):15-18.
- Ellis R, Ellis C. Dog and cat bites. Am Fam Physician. 2014;90(4):239-243.
- Aziz H, Rhee P, Pandit V, et al. The current concepts in management of animal (dog, cat, snake, scorpion) and human bite wounds. J Trauma Acute Care Surg. 2015;78(3):641-648.
- Hon K-L, Fu C-C, Chor C-M, et al. Issues associated with dog bite injuries in children and adolescents assessed at the emergency department. Pediatr Emerg Care. 2007;23(7):445-449.
- Basco AN, McCormack ER, Basco WT Jr. Age- and sex-related differences in nonfatal dog bite injuries among persons aged 0-19 treated in hospital emergency departments, United States, 2001-2017. Public Health Rep. 2020;135(2):238-244.
- Ramgopal S, Macy ML. U.S. estimates for dog bite injuries presenting to emergency departments. Public Health. 2021;196:1-3.
- Parikh UM, Mentz J, Collier I, et al. Strategies to minimize surgical scarring: Translation of lessons learned from bedside to bench and back. Adv Wound Care (New Rochelle). 2022;11(6):311-329.
- Gantwerker EA, Hom DB. Skin: Histology and physiology of wound healing. Clin Plast Surg. 2012;39(1):85-97.
- Zoppo G, Marrone F, Pittarello M, et al. AI technology for remote clinical assessment and monitoring. J Wound Care. 2020;29(12):692-706.
- Jaman J, Martić K, Rasic N, et al. Is the use of specific time cut-off or “golden period” for primary closure of acute traumatic wounds evidence based? A systematic review. Croat Med J. 2021;62(6):614-622.
- Baker MD, Lanuti M. The management and outcome of lacerations in urban children. Ann Emerg Med. 1990;19(9):1001-1005.
- Quinn JV, Polevoi SK, Kohn MA. Traumatic lacerations: What are the risks for infection and has the ‘golden period’ of laceration care disappeared? Emerg Med J. 2014;31(2):96-100.
- Kimberlin DW, Banerjee R, Barnett ED, et al. Tetanus (Lockjaw). Red Book: 2024–2027 Report of the Committee on Infectious Diseases. 33rd ed. American Academy of Pediatrics;2024:848-853.
- Centers for Disease Control and Prevention. Child and adolescent immunization schedule by age. Updated Nov. 21, 2024. https://www.cdc.gov/vaccines/hcp/imz-schedules/child-adolescent-age.html
- Drapkin Z, Madsen TE, Weaver N, et al. Accuracy of parental-reported tetanus vaccination status for children with lacerations. Pediatr Emerg Care. 2021;37(10):e640-e644.
- Zeretzke-Bien C, McCall J, Wylie T, et al. Using an online vaccination registry to confirm tetanus status in children with tetanus-prone wounds. West J Emerg Med. 2020;21(5):1140-1146.
- Centers for Disease Control and Prevention. Clinical guidance for wound management to prevent tetanus. Updated Aug. 15, 2024. https://www.cdc.gov/tetanus/hcp/clinical-guidance/index.html
- Fielding P, Messahel S. Guideline review — human and animal bites: Antimicrobial prescribing. Arch Dis Child Educ Pract Ed. 2022;107(6):442-445.
- Rothe K, Tsokos M, Handrick W. Animal and human bite wounds. Dtsch Arztebl Int. 2015;112(25):433-443.
- Tabaka ME, Quinn JV, Kohn MA, et al. Predictors of infection from dog bite wounds: Which patients may benefit from prophylactic antibiotics? Emerg Med J. 2015;32(11):860-863.
- Pieracci EG, Pearson CM, Wallace RM, et al. Vital signs: Trends in human rabies deaths and exposures — United States, 1938-2018. MMWR Morb Mortal Wkly Rep. 2019;68(23):524-528.
- Kimberlin DW, Banerjee R, Barnett ED, et al, eds. Rabies. Red Book: 2024–2027 Report of the Committee on Infectious Diseases. 33rd ed. American Academy of Pediatrics;2024:702-710.
- Liu C, Cahill JD. Epidemiology of rabies and current U.S. vaccine guidelines. R I Med J (2013). 2020;103(6):51-53.
- Gibbons K, Dvoracek K. Rabies postexposure prophylaxis: What the U.S. emergency medicine provider needs to know. Acad Emerg Med. 2023;30(11):1144-1149.
- Centers for Disease Control and Prevention. Rabies post-exposure prophylaxis. Updated June 20, 2024. https://www.cdc.gov/rabies/hcp/prevention-recommendations/post-exposure-prophylaxis.html
- Young KD. Pediatric procedural pain. Ann Emerg Med. 2005;45:160–171.
- Siembieda J, Heyming T, Padlipsky P, et al. Triple versus single application of lidocaine, epinephrine, and tetracaine for laceration repair in children. Pediatr Emerg Care. 2022; 38(2):e472-e474.
- Mace SE, Ulintz A, Peterson B, et al. Fifteen years’ experience with safe and effective procedural sedation in infants and children in a general emergency department. Pediatr Emerg Care. 2021;37(9):e500-e506.
- Mace SE, Whiteman P, Avarello JT, et al. Local and topical anesthetics for pediatric patients in the emergency department. Pediatr Emerg Care. 2020;36(12):593-601.
- Kouba DJ, LoPiccolo MC, Alam M, et al. Guidelines for the use of local anesthesia in office-based dermatologic surgery. J Am Acad Dermatol. 2016;74(6):1201-1219.
- Ilicki J. Safety of epinephrine in digital nerve blocks: A literature review. J Emerg Med. 2015;49(5):799-809.
- Ciavola L, Sogni F, Mucci B, et al. Analgosedation in pediatric emergency care: A comprehensive scoping review. Pharmaceuticals (Basel). 2024;17(11):1506.
- Del Pizzo J, Fein J. Oral ketamine and midazolam for procedural sedation in the pediatric emergency department. Pediatr Emerg Care. 2025;41(2):122-126.
- Carlone G, Trombetta A, Amoroso S, et al. Intramuscular dexmedetomidine, a feasible option for children with autism spectrum disorders needing urgent procedural sedation. Pediatr Emerg Care. 2019;35(6):e116-e117.
- Azak M, Aksucu G, Çağlar S. The effect of parental presence on pain levels of children during invasive procedures: A systematic review. Pain Manag Nurs. 2022;23(5):682-688.
- Romito B, Jewell J, Jackson M; AAP Committee on Hospital Care; Association of Child Life Professionals. Child life services. Pediatrics. 2021;147(1):e2020040261.
- Choi H, Kim H. Efficacy of cartoons as a distraction technique for children undergoing suture of facial lacerations in the emergency department. Pediatr Emerg Care. 2021;37(9):471-473.
- McEvoy AO, Vincent OB, Vazifedan T, et al. Virtual reality as active distraction in laceration repair: A game changer? Pediatr Emerg Care. 2025;41(3):208-212.
- Thompson DG, Tielsch-Goddard A. Improving management of patients with autism spectrum disorder having scheduled surgery: Optimizing practice. J Pediatr Health Care. 2014;28(5):394-403.
- Huang CY, Choong MY. Comparison of wounds’ infection rate between tap water and normal saline cleansing: A meta-analysis of randomised control trials. Int Wound J. 2019;16(1):300-301.
- Holman M. Using tap water compared with normal saline for cleansing wounds in adults: A literature review of the evidence. J Wound Care. 2023;32(8):507-512.
- Coccolini F, Sartelli M, Sawyer R, et al. Antibiotic prophylaxis in trauma: Global Alliance for Infection in Surgery, Surgical Infection Society Europe, World Surgical Infection Society, American Association for the Surgery of Trauma, and World Society of Emergency Surgery guidelines. J Trauma Acute Care Surg. 2024;96(4):674-682.
- Tan YY, Chua ZX, Loo GH, et al. Risk of wound infection with use of sterile versus clean gloves in wound repair at the emergency department: A systematic review and meta-analysis. Injury. 2023;54(11):111020.
- Zwaans JJM, Raven W, Rosendaal AV, et al. Non-sterile gloves and dressing versus sterile gloves, dressings and drapes for suturing of traumatic wounds in the emergency department: A non-inferiority multicentre randomised controlled trial. Emerg Med J. 2022;39(9):650-654.
- Adl H, Henkelman E, Goldman RD. Topical skin adhesives for laceration repair in children. Can Fam Physician. 2021;67(4):260-262.
- Quinn JV, Drzewiecki A, Li MM, et al. A randomized controlled trial comparing a tissue adhesive with suturing in the repair of pediatric facial lacerations. Ann Emerg Med. 1993;22:1130-1135.
- Otterness K, Thode HC Jr, Singer AJ. Methods of laceration closure in the ED: A national perspective. Am J Emerg Med. 2020;38(6):1058-1061.
- Hock MO, Ooi SB, Saw SM, et al. A randomized controlled trial comparing the hair apposition technique with tissue glue to standard suturing in scalp lacerations (HAT study). Ann Emerg Med. 2002;40(1):19-26.
- Munns E, Kienstra A, Combs P, et al. Cosmetic outcomes of simple pediatric facial lacerations repaired with skin adhesive compared with skin adhesive with underlying adhesive strips. Pediatr Emerg Care. 2022;38(10):477-480.
- Preiksaitis C. Suture materials. CORE EM. Published Nov. 8, 2017. https://coreem.net/core/suture-materials/
- Edwards S, Parkinson L. Is fixing pediatric nail bed injuries with medical adhesives as effective as suturing? Pediatr Emerg Care. 2019;35(1):75-77.
- Lin B. Trick of the trade: Dermal avulsion injuries 2.0. Academic Life in Emergency Medicine. Published Nov. 5, 2015. https://www.aliem.com/trick-of-trade-dermal-avulsion-injuries-2-0/
- Beatty R. How to manage fingertip avulsions. Provider Practice Essentials. Published Aug. 15, 2024. https://ppemedical.com/blog/how-to-manage-fingertip-avulsions/
- Stratis C, Haider SA, Oleru O, et al. Paper tape may improve scar aesthetics and prevent wound closure complications. Plast Aesthet Nurs (Phila). 2024;44(1):59-69.
- O’Brien L, Jones DJ. Silicone gel sheeting for preventing and treating hypertrophic and keloid scars. Cochrane Database Syst Rev. 2013;2013(9):CD003826.
- Tran B, Wu JJ, Ratner D,et al. Topical scar treatment products for wounds: A systematic review. Dermatol Surg. 2020;46(12):1564-1571.
- Draelos ZD, Rizer RL, Trookman NS. A comparison of postprocedural wound care treatments: Do antibiotic-based ointments improve outcomes? J Am Acad Dermatol. 2011;64(3 Suppl):S23-S29.
- Tandon S, Smale M, Pacilli M, et al. Tissue adhesive and adhesive tape for pediatric wound closure: A systematic review and meta-analysis. J Pediatr Surg. 2021;56(5):1020-1029.
- Barton MS, Chaumet MSG, Hayes J, et al. A randomized controlled comparison of guardian-perceived cosmetic outcome of simple lacerations repaired with either Dermabond, Steri-Strips, or absorbable sutures. Pediatr Emerg Care. 2024;40(10):700-704.
- Miller A, Levy J, Lyons T. Surgical specialty consultation for pediatric facial laceration repair. Pediatr Emerg Care. 2024;40(8):e120-e125.
- Amanullah S, Linakis JG, Vivier PM, et al. Differences in presentation and management of pediatric facial lacerations by type of health insurance. West J Emerg Med. 2015;16:527–534.
- Okoniewski W, Sundaram M, Chaves-Gnecco D, et al. Culturally sensitive interventions in pediatric primary care settings: A systematic review. Pediatrics. 2022;149(2):e2021052162.
- Brotanek JM, Seeley CE, Flores G. The importance of cultural competency in general pediatrics. Curr Opin Pediatr. 2008;20(6):711-718.
- Olness K, Torjesen K. Providing culturally effective care. In: McInerny TK, Adam HM, Campbell DE, et al, eds. American Academy of Pediatrics Textbook of Pediatric Care. 2nd ed. American Academy of Pediatrics;2016:349-367.