
Clinical Approach to Pediatric Shoulder Injuries
October 1, 2025
By Jonathon Stewart, MD, and Vincent Marsh, MD, FACEP, Maj ANG
Executive Summary
- The median prevalence of shoulder injuries in youth sports is approximately 11%.
- Acute injuries are more common in contact sports, while overuse injuries occur in sports characterized by repetitive motions, such as baseball, softball, and tennis.
- Predisposing factors linked to an increased risk of shoulder injuries in youth include muscular weakness with external or internal rotation, scapular dyskinesia, strength imbalances between the sides of the body, and restricted range of motion.
- The supraspinatus muscle, responsible for initiating shoulder abduction, is tested using the “empty can” or Jobe test.
- The infraspinatus and teres minor muscles, responsible for external rotation and stabilization of the shoulder, are tested using the external rotation test.
- The subscapularis muscle, responsible for internal rotation and stabilization of the shoulder, is tested using the “lift-off” or Gerber test.
- The apprehensive test is used to evaluate the anterior glenohumeral joint.
- The Hawkins-Kennedy and Neer tests are used to assess rotator cuff irritation or impingement.
Epidemiology
Pediatric shoulder injuries represent a significant clinical concern, particularly as millions of youth engage in sports activities that heighten their risk for such injuries. A systematic review and meta-analysis of youth sports-related shoulder injuries found that the median seasonal prevalence of shoulder injuries was 10.9%, with a range from 1.2% to 28.2%.1 Acute traumatic shoulder injuries are observed frequently in contact sports, including hockey, wrestling, rugby, football, and soccer, where high-impact collisions are common. Conversely, non-contact or overuse injuries predominantly occur in sports characterized by repetitive motions, such as baseball, softball, and tennis.1
The spectrum of common shoulder injuries in this population includes muscle and tendon strains, tears, ligamentous sprains and ruptures, rotator cuff injuries, labral injuries, acromioclavicular joint separations, humeral dislocations, as well as fractures of the humerus, clavicle, or scapula. These injuries can have significant implications, leading to time lost from sport-specific training and competitions, disrupted sleep patterns from pain, and acute or chronic discomfort that may affect day-to-day activities. Consequently, understanding the epidemiology of shoulder injuries in pediatric athletes is crucial for developing effective prevention and management strategies.1
Etiology
The etiology of pediatric shoulder injuries typically is multifactorial, involving various risk factors and mechanisms of injury. The previously mentioned systematic review of 97 studies on sports-related shoulder injuries in young athletes identified several key causative factors. Notably, shoulder injuries are more frequently observed during competition compared to practice or training sessions.1
The most common mechanisms leading to injury include collisions with other players or contact with environmental objects, particularly prevalent in contact sports like hockey and rugby. Additionally, certain predisposing conditions have been linked to an increased risk of shoulder injuries in youth athletes. These include muscular weakness in both external and internal rotation, scapular dyskinesia, strength imbalances between the sides of the body, and restricted range of motion. An increase in training load, particularly when exceeding a 60% rise relative to previous months, also has been highlighted as a significant risk factor.1
Scapular dyskinesia is characterized by abnormal scapular movement patterns and also is recognized as an independent risk factor. It typically manifests as changes in scapular positioning and motion during arm elevation and lowering, which can compromise shoulder stability and function.2-5 An example of this includes repetitive overhead throwing, causing the affected scapula to wing out and tip forward instead of gliding smoothly along the rib cage.6
A 2025 systematic review of risk factors for shoulder injuries in female athletes playing overhead sports also identified six key risk factors for injury.7 The most common sport linked to injury was volleyball, followed by softball, swimming, and gymnastics. Significant risk factors include dominant shoulder involvement, overuse volume, prior injuries, increased age at injury, and multidirectional instability. Overhead athletes tend to exhibit greater external rotation and reduced internal rotation in the dominant shoulder, which may contribute to injury risk.7
Pathophysiology
The pathophysiology of shoulder injuries in children compared to adults is primarily influenced by the anatomical differences between the two groups. The presence of growth plates plays a crucial role; injuries to these areas can disrupt normal growth patterns and lead to deformities if not managed properly.
The growth plate, also termed the physis, is a cartilaginous area of the bone that is responsible for longitudinal growth. The epiphysis is the very proximal or distal part of the bone, which articulates with the epiphysis of another bone to form a joint. An apophysis is an epiphysis that does not articulate with another bone. The diaphysis of a bone is the mid-section part of the long bone. The metaphysis is the part of the diaphysis that is adjacent to the physis. This part of the bone is active with cell division and growth. Finally, the periosteum is the membrane that lines the outer surface of all bones except at the joint. (See Figure 1.)
Figure 1. Physeal Growth Plate |
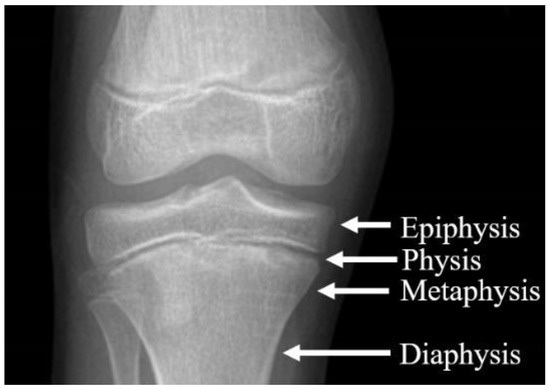 |
Source: Frydrýšek K, Čepica D, Halo T, et al. Biomechanical analysis of staples for epiphysiodesis. Applied Sciences. 2022;12(2):614. |
Intramembranous ossification is the process that occurs when mesenchymal cells (multipotent stem cells capable of differentiating into various cell types, including bone, cartilage, fat, and muscle cells) differentiate directly into osteoblasts, forming bone without a cartilage model. It primarily contributes to the formation of the clavicle.8
Endochondral ossification involves the formation of a cartilage model first, which then is replaced by bone. It is responsible for the development of the scapula and the humeral head.8 Primary ossification develops around the sixth to seventh week of gestation, leading to the formation of the diaphysis of long bones. They are crucial for the initial bone structure.8 Secondary ossification centers appear later and are located at the ends of bones (epiphysis) and are involved in growth in length and width. They are cartilaginous at birth and gradually ossify postnatally.8
The shoulder itself is primarily composed of osseous structures between the humerus, clavicle, and scapula. Articulations of these structures form joints, including the glenohumeral joint, acromioclavicular joint (AC joint), and the sternoclavicular joint. Additionally, soft tissue and muscular components are key areas of the shoulder that provide stability, facilitate movement, and protect structures within the joint. These include the muscles and tendons of the rotator cuff, which are the supraspinatus, infraspinatus, subscapularis, and teres minor. Ligaments that provide passive stability and connect bones include the coracohumeral ligament, glenohumeral ligament, and coracoacromial ligament.
The humerus undergoes ossification through endochondral ossification, starting in utero around 8 to 10 weeks of gestation. The humeral shaft ossifies first, while the proximal and distal ends remain cartilaginous at birth. The proximal humerus develops three secondary ossification centers: the humeral head, the greater tuberosity (by about 10 months), and the lesser tuberosity (fusing by around 5 years of age). The humeral head shows early pre-ossification centers within the first few months after birth, with complete fusion of ossification centers occurring by late puberty (around 15 to 20 years of age).
The scapula undergoes complex ossification beginning around the 11th week of gestation, with only the body ossified at birth while the remaining parts, including the glenoid and coracoid process, stay cartilaginous. It features multiple ossification centers; the subcoracoid center appears between 8 and 10 years and fuses by 16 to 17 years, while inferior glenoid centers emerge around 14 to 15 years and complete fusion by 17 to 19 years. The coracoid process has ossification centers at its body, base, and tip, appearing sequentially from birth to age 14 years, and the acromion has two to five centers that begin around 15 to 18 years of age. Overall, the scapula’s ossification and fusion processes culminate by approximately 15 to 16 years of age.
The clavicle is unique in its ossification process, beginning as the first bone to ossify in the human fetus at approximately 5 to 6 weeks of gestation. Its ossification occurs through both intramembranous and endochondral methods, with the midportion ossified at birth and the medial and lateral ends remaining cartilaginous. Initial ossification centers extend toward the acromion and fuse shortly after birth. Secondary ossification centers develop at both ends postnatally, with the medial center typically appearing and fusing between ages 11 to 25 years, while the lateral end remains cartilaginous for longer. The clavicle’s growth and maturation continue into early adulthood, completing its fusion process by around 25 years of age, making it the last bone to fully mature despite being the first to start ossification.8
Fractures involving the growth plate can disrupt normal bone growth, leading to limb length discrepancies or angular deformities if not accurately diagnosed or treated. There are five types of Salter-Harris fractures, categorized based on the pattern of the fracture and its relation to the growth plate. (See Table 1.)
Table 1. Salter Harris Classification |
Type I
Type II
Type III
Type IV
Type V
|
Adapted from: Levine RH, Thomas A, Nezwek TA, Waseem M. Salter-Harris Fracture. In: StatPearls. StatPearls Publishing; Aug. 10, 2023. |
Clinical Evaluation
The examination of the pediatric shoulder begins after a thorough primary survey has been completed, assuring there are no acute life threats that would take precedence to a musculoskeletal shoulder injury.9 After this, next steps include gathering details about the onset of symptoms, mechanism of injury (e.g., fall on an outstretched hand), activity level, and any previous shoulder injuries. It is essential to assess the nature of the pain, including its location, intensity, duration, and any accompanying symptoms, such as weakness or instability.
Following the history, a visual inspection is conducted to look for swelling, bruising, deformity, or asymmetry, with the patient appropriately attired to expose the shoulder. The examination continues with palpation of shoulder structures, including the acromioclavicular joint, glenohumeral joint, biceps tendon, and surrounding muscles to assess for tenderness, warmth, crepitus, or bony irregularities.10-12
Range of motion then is evaluated for both active and passive movements in all directions: abduction, adduction, flexion, extension, and internal and external rotation, noting any limitations or pain experienced during these actions. Strength testing follows, focusing on the major muscle groups, including the supraspinatus, infraspinatus, teres minor, and subscapularis, to determine strength and stability.
Special tests are conducted to assess for specific conditions, such as instability, impingement, or AC joint injuries. The apprehension test, Hawkins-Kennedy test, Neer test, and cross-arm test commonly are used to identify pathology, looking for signs like apprehension or pain. Finally, a neurovascular assessment ensures that neurological function — specifically axillary nerve integrity — is intact, alongside the evaluation of blood flow to the limb to rule out vascular compromise.10-12
The supraspinatus is primarily responsible for initiating shoulder abduction —lifting the arm laterally away from the body — and helps maintain the head of the humerus within the glenoid cavity. Its function can be evaluated through strength testing using the “empty can” or Jobe test, where the arm first is abducted to 90 degrees. This is followed by the patient making a fist with the thumb sticking out and internally rotating the shoulder with the thumb pointing down to the floor. The arm then is angled forward at a 30-degree forward angle. The examiner then pushes down noting pain or weakness, which may indicate a tear or impingement affecting the supraspinatus muscle. (See Figure 2.)
Figure 2. Empty Can or Jobe Test |
 |
Source: Brown G, Park K, Bicknell RT. Management of occupational shoulder injuries in primary care. J Musculoskelet Disord Treat. 2015;1:002. Open Access Creative Commons license. https://www.clinmedjournals.org/articles/jmdt/journal-of-musculoskeletal-disorders-and-treatment-jmdt-1-002.php |
The infraspinatus is crucial for external rotation of the shoulder and stabilizes the shoulder joint during various movements. To assess its strength, clinicians typically perform an external rotation test, with the arm at the side and the elbow flexed at 90 degrees, where the patient resists an inward force applied by the examiner. Pain or significant weakness can suggest an infraspinatus tear or related pathology.10-12
Teres minor serves a similar function to infraspinatus, assisting with external rotation and stabilization of the shoulder, although it often is evaluated along with infraspinatus because of their overlapping roles. The subscapularis is responsible for internal rotation and stabilization of the glenohumeral joint, typically tested through the lift-off test or Gerber test. In this test, the patient places their hand on the mid-lumbar spine with the palm facing out and is asked to lift their hand away from the back. Inability to do so or pain during this movement may indicate a subscapularis injury.10-12
Apprehension testing is an additional clinical maneuver used to evaluate the anterior glenohumeral. The test is performed with the patient lying supine, the arm abducted to 90 degrees, and the elbow flexed at 90 degrees. The examiner applies an external rotation force to the humerus, pushing the humeral head anteriorly, which stresses the anterior capsule and labrum. A positive apprehension test occurs when the patient exhibits apprehension or discomfort, expressing a sensation that the shoulder might dislocate or “give way.” This reaction is characterized not merely by pain but by visible anxiety or resistance to further external rotation because of fear of instability, indicating insufficiency or injury to the shoulder’s anterior stabilizing structures. The apprehension test often precedes the relocation test, where a posteriorly directed force on the anterior glenohumeral joint alleviates the patient’s apprehension, thereby confirming anterior instability.10-12
Additionally, special tests such as the Hawkins-Kennedy and Neer tests are commonly used clinical maneuvers to assess for rotator cuff impingement and related shoulder pathology in pediatric and adolescent patients. The Hawkins-Kennedy test is performed with the shoulder flexed to 90 degrees and the elbow bent at 90 degrees, followed by passive internal rotation of the arm by the examiner. (See Figure 3.) A positive test elicits pain during this motion, indicating impingement of the rotator cuff tendons, particularly the supraspinatus, beneath the coracoacromial arch.
Figure 3. Hawkins-Kennedy Test |
 |
Source: Brown G, Park K, Bicknell RT. Management of occupational shoulder injuries in primary care. J Musculoskelet Disord Treat. 2015;1:002. Open Access Creative Commons license. https://www.clinmedjournals.org/articles/jmdt/journal-of-musculoskeletal-disorders-and-treatment-jmdt-1-002.php |
Neer test involves passively flexing the patient’s arm overhead while the arm is internally rotated. Pain during this motion suggests irritation or impingement of the rotator cuff tendons against the anterior acromion.10-12 (See Figure 4.)
Figure 4. Neer Test |
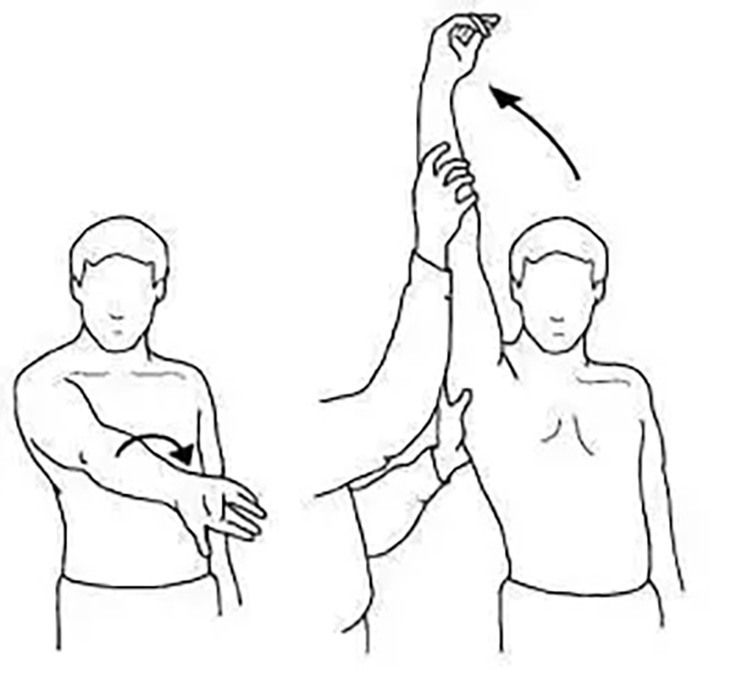 |
Source: https://commons.wikimedia.org/wiki/File:Neer_Test.jpg |
Diagnostic Studies
When evaluating orthopedic trauma and injury, multiple diagnostic studies often play a pivotal role in accurately diagnosing injury and guiding treatment. The initial assessment usually begins with obtaining plain film imaging. X-rays provide rapid assessment of osseous structures to evaluate for pathology, including fractures, dislocations, or traumatic subluxations. This imaging is most accessible given the wide availability in most healthcare settings.
Plain films are a practical first choice because of their speed, relative availability, and cost when compared to other imaging modalities.13 Furthermore, the radiation dose of plain X-rays is lower compared to computed tomography (CT) imaging, making them safer for evaluating children. Shoulder X-rays typically deliver an effective radiation dose of approximately 0.01 millisieverts (mSv) to 0.1 mSv per examination. In contrast, shoulder CT scans expose patients to significantly higher radiation doses, generally in the range of 1 mSv to 2 mSv per scan — approximately 10 to 100 times greater than that of X-rays.14-15
However, there are drawbacks to plain films, including less effective visualization and diagnosis of soft tissue injuries. These can include ligament and tendon damage, which may accompany fractures. Additionally, the open growth plates can be challenging to assess. Some injuries may not be evident on plain X-rays, leading to potential misdiagnosis of certain fractures or growth plate injuries. Furthermore, some injuries, such as stress fractures or occult fractures, may not be visible on X-rays.13,16
To complement plain imaging, advanced techniques such as CT may be employed to obtain high-resolution, cross-sectional imaging, which allows for detailed assessment of complex fractures. This is particularly useful in complex anatomical areas such as the shoulder where overlap of bony structures may make identification of injury more difficult. As mentioned earlier, CT is valuable in detecting occult fractures and injury to growth plates that may be missed initially on plain radiographs. There are additional considerations and drawbacks to CT imaging, including greater exposure to ionizing radiation, which increases long-term risk for malignancy. The cost of CT imaging also is a considerable drawback when compared to plain films. Last, while CT improves visualization of bony injuries, it is not as effective as magnetic resonance imaging (MRI) for assessing soft tissue injuries.16
MRI is a valuable diagnostic tool for evaluating pediatric shoulder injuries. One of the primary advantages of MRI is its ability to produce high-resolution images of soft tissues, including muscles, tendons, ligaments, and cartilage, without exposing young patients to ionizing radiation, which is of particular importance because of radiation effects over their lifetime. Moreover, MRI can provide detailed insights into conditions such as rotator cuff tears, labral injuries, and other soft tissue abnormalities that may not be visible on conventional X-rays.17
However, MRI also has its drawbacks. Limitations include the need for patient cooperation and limited allowance for patient movement, which can be challenging for younger children or those with anxiety or claustrophobia, potentially necessitating sedation in some cases.18-19 Additionally, the availability and cost of MRI may pose practical challenges, since not all facilities have immediate access to this imaging modality, and it may not be covered by all insurance plans. There also is a risk of artifacts or misinterpretations in pediatric patients because of their smaller anatomy and propensity for movement.
Ultrasound can play a useful role in the imaging of pediatric musculoskeletal injuries because of its many advantageous features. It is an easy-to-use, widely available, cost-effective, and radiation-free modality, which makes it particularly suitable for children, such as young athletes recovering from trauma who often require multiple follow-up examinations. Ultrasound allows real-time, dynamic assessment of soft tissue structures, including tendons, ligaments, and muscles, offering an interactive approach where the user can precisely locate and evaluate the area of injury while also performing comparative studies with the contralateral side.
However, ultrasound does have limitations, including its strong dependence on the operator’s expertise and experience. Thus, proficiency and thorough understanding of pediatric musculoskeletal anatomy and injury mechanisms are critical to maximizing the diagnostic yield of ultrasound in these settings. Overall, ultrasound can be an essential first-line or complementary imaging technique in the pediatric population, especially for superficial structures and in situations where radiation exposure from X-rays and CT scans should be minimized.20
Differential Diagnosis
The differential diagnosis of pediatric shoulder injury is broad and must be tailored to the child’s age, mechanism of injury, and skeletal maturity. In younger children, injuries often involve the growth plates or metaphyseal bone, while older adolescents may present with soft tissue injuries or true joint instability similar to adult patterns.21
A common diagnosis in all age groups is clavicle fracture, most often involving the midshaft and resulting from a fall onto the shoulder.22 Proximal humeral fractures also frequently are encountered, particularly in younger children. These often involve the physis and typically heal well without surgical intervention because of the significant remodeling capacity of the proximal humerus.
Scapular fractures in the pediatric population, although rare, represent a significant component of shoulder trauma following blunt chest injury. These fractures often occur alongside other serious shoulder and thoracic injuries, reflecting high-energy mechanisms that can affect multiple structures within the shoulder girdle. Fonacier et al found that pediatric patients with scapular fractures frequently sustain additional fractures and intrathoracic injuries, such as pulmonary contusions, pneumothorax, and rib fractures, indicating that scapular fractures may serve as markers for more extensive trauma.23
Physeal and apophyseal injuries are especially relevant in pediatric athletes.24 Little League shoulder, or proximal humeral epiphysiolysis, is a common overuse injury in adolescent baseball players. It results from repetitive throwing stress and presents with gradual-onset pain and tenderness.25 Imaging reveals widening of the proximal humeral growth plate, and MRI may show associated marrow edema or early stress changes.26 Similar apophyseal injuries may affect the acromion or coracoid, particularly in adolescents engaged in overhead sports, and may present with localized tenderness and activity-related pain.
AC joint injury in children and adolescents also is a consideration following a direct fall onto the shoulder. In younger athletes, such injuries are more likely to result in lateral clavicle physeal or metaphyseal fractures rather than pure ligamentous damage. Clinically, patients typically present with localized swelling and tenderness over the AC joint, and more severe injuries may demonstrate a noticeable deformity.10,27
Shoulder dislocations, while rare in young children because of the relative strength of soft tissues, becomes more common during adolescence. The most frequent type is anterior glenohumeral dislocation, which typically occurs after forceful abduction and external rotation. Posterior dislocations, although rare, may result from seizures, electrical injury, or, in a case reported by Park et al, a high-energy injury secondary to a dirt bike injury.28 These events can be associated with labral injuries such as Bankart lesions, anterior labral periosteal sleeve avulsion (ALPSA) lesions, and Hill-Sachs deformities.29-31
A Bankart lesion involves a tear of the antero-inferior labrum of the glenoid — the fibrocartilaginous rim that stabilizes the shoulder joint by deepening the socket. This lesion occurs when the humeral head is forcibly dislocated anteriorly, causing the labrum to detach from the glenoid rim and leading to compromised stability of the shoulder.30,31
The Hill-Sachs deformity, often seen concurrently with a Bankart lesion, is an impaction fracture on the posterolateral aspect of the humeral head. (See Figure 5.) It happens when the dislocated humeral head impacts against the anterior glenoid rim during the dislocation event, resulting in a compression fracture. Together, the Bankart lesion and Hill-Sachs deformity contribute to greater joint instability and can make recurrent anterior shoulder dislocations more likely.30,31
Figure 5. Shoulder Dislocation with Bankart and Hill-Sachs Lesion, Before and After Reduction |
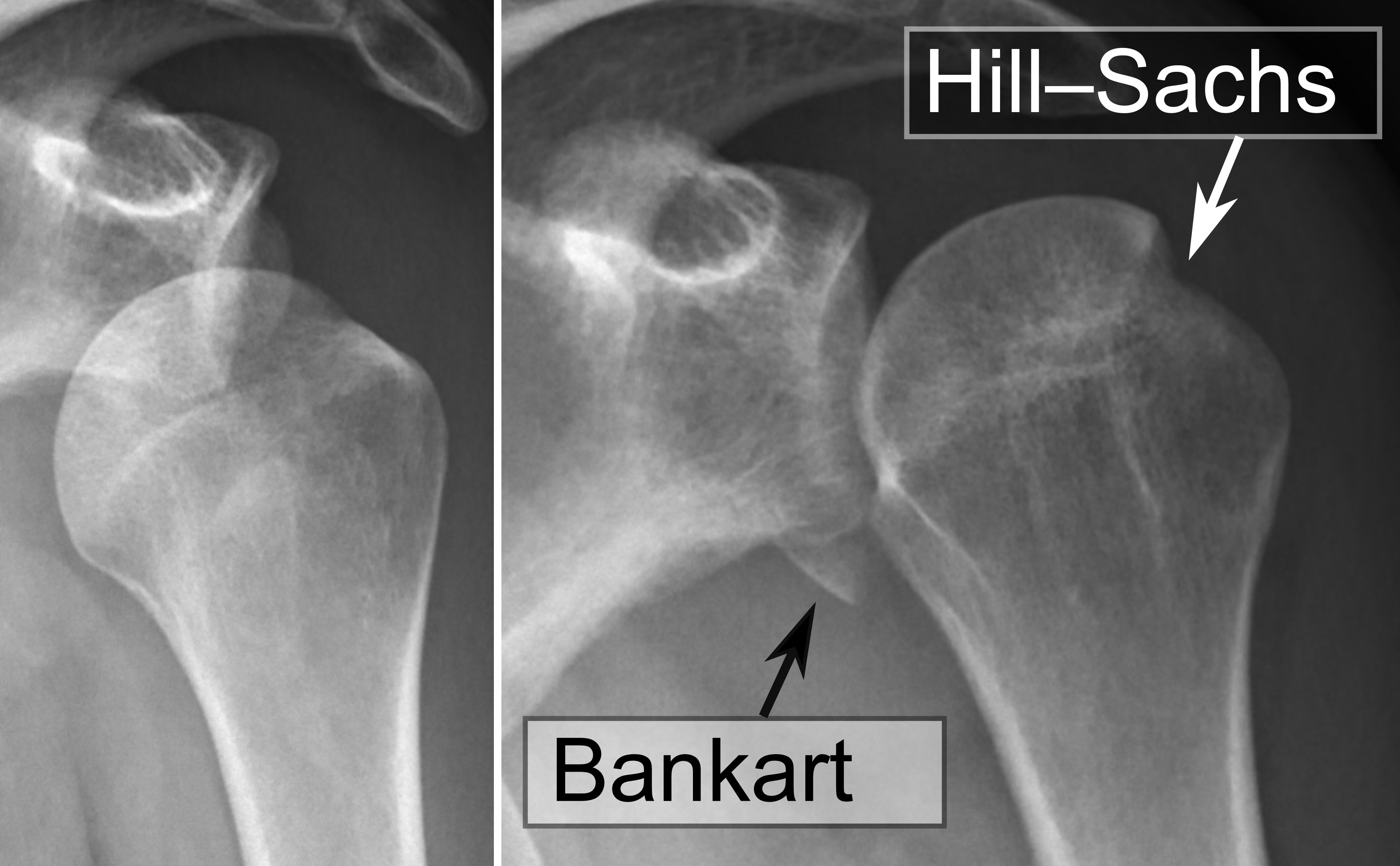 |
Source: Mikael Häggström |
An ALPSA lesion is an additional soft tissue injury seen in shoulder dislocation cases, particularly in younger patients. It involves the detachment of the anterior labrum along with the periosteal sleeve from the glenoid rim. This periosteal sleeve remains intact but is displaced medially and inferiorly, leading to a medialized labral lesion. This displacement prevents the labrum from functioning effectively as a stabilizer, contributing to ongoing shoulder instability.32
Multidirectional instability (MDI) is another entity, seen more commonly in hypermobile adolescents and often presenting with vague, chronic shoulder discomfort without a clear history of trauma. MDI of the shoulder is a complex condition characterized by instability of the shoulder joint in two or more planes of motion. Unlike instability caused by a single traumatic event, MDI often involves generalized looseness or laxity of the joint structures, leading to excessive movement of the humeral head within the glenoid socket.
MDI may develop primarily through two mechanisms: repetitive microtrauma seen commonly in overhead athletes (e.g., baseball pitchers, volleyball players, gymnasts, swimmers), leading to capsular and ligamentous laxity, or through systemic disorders causing generalized ligamentous hyperlaxity such as Ehlers-Danlos syndrome, Marfan syndrome, osteogenesis imperfecta, and benign joint hypermobility syndrome. Clinically, MDI is defined as instability occurring in two or more directions of the shoulder joint without a significant traumatic event, often presenting with symptoms related to the imbalance between shoulder mobility and stability.33
Finally, an unfortunate and cannot-miss diagnosis includes nonaccidental trauma (NAT). Symptoms that suggest NAT in children differ from those typically seen in accidental injuries. One of the key indicators of NAT is the presence of bruising in non-ambulatory children, since infants who are not yet mobile rarely sustain accidental bruises. Additionally, bruises located on soft tissue areas, such as the cheeks, ears, neck, buttocks, and trunk, are more suspicious for abuse, especially when multiple bruises are in various stages of healing, indicating repeated injuries over time. Sentinel injuries, which are minor but concerning signs such as bruising or intraoral lesions, often precede more severe abuse and warrant prompt investigation. Skeletal injuries further aid in distinguishing NAT from accidental trauma. Multiple fractures at various stages of healing or fractures inconsistent with the child’s developmental abilities and the history provided — such as rib fractures or scapular fractures — are highly concerning for abuse. Additional signs include traumatic hair loss due to pulling, inconsistent caregiver explanations, or a delay in seeking medical care.34
In contrast, accidental injuries typically are consistent with the child’s developmental level, such as bruises found on bony prominences common in ambulatory children and injuries resulting from witnessed falls or accidents. These injuries usually present as isolated events without the presence of multiple injuries in differing stages of healing. A coherent and plausible history that aligns with the injury pattern also is more common in accidental trauma.34
Management
The management of pediatric shoulder injuries resulting from trauma is a systematic process that begins with an immediate assessment and continues through diagnosis, treatment, and rehabilitation. Incorporating the principles of Advanced Trauma Life Support (ATLS) is essential in the initial management of pediatric shoulder injuries resulting from trauma.
The ATLS framework emphasizes a systematic approach that begins with a primary survey following the ABCDE method. First, assess the airway (A) to ensure it is clear and secure, checking for any signs of obstruction. Next, evaluate breathing (B) to confirm adequate ventilation, observing for respiratory distress and auscultating breath sounds to rule out possible complications, such as pneumothorax or hemothorax, which may occur alongside shoulder injuries. The circulation (C) assessment involves monitoring vital signs, checking for significant bleeding, and ensuring adequate perfusion; this may include establishing vascular access and administering volume resuscitation as needed. Following that, conduct a rapid neurological assessment (D) using the Glasgow Coma Scale (GCS) to evaluate consciousness and check for any signs of limb weakness, numbness, or altered sensation that could indicate neurological injury. Finally, during the exposure phase (E), fully undress the patient to identify any other injuries while taking care to prevent hypothermia. After stabilization, a secondary survey allows for a comprehensive physical examination focused on additional injuries and for the purpose of this paper, the shoulder.9
Conservative management often is the first approach for less severe injuries. This typically includes the application of ice to reduce swelling, the use of a sling or immobilizer to limit movement and provide support, and the administration of analgesics for pain relief.10
The management of Little League shoulder primarily involves resting from overhead throwing activities for three to six months until symptoms resolve, preventing progression to more severe injury, such as a stress fracture of the proximal humeral growth plate. Once the pain subsides, patients should begin a structured rehabilitation program focusing on core and rotator cuff strengthening exercises, followed by a gradual return to throwing under supervision, ideally with the involvement of a physical therapist.
Prevention strategies include adhering to age-based pitch count limits, ensuring adequate rest periods, which ideally should include taking one season off from throwing per year, and promoting proper throwing biomechanics to reduce shoulder stress. It also is recommended to avoid the use of nonsteroidal anti-inflammatory drugs (NSAIDs) before throwing to prevent masking underlying inflammation and pain. In uncomplicated cases, consultation with sports medicine or orthopedic specialists may not be necessary when clinicians are confident in the diagnosis and treatment plan.35
Pediatric proximal humerus fractures are managed through either nonoperative or operative approaches, with the treatment choice largely guided by the patient’s age, fracture displacement, and the presence of associated injuries. Nonoperative management is the mainstay for the majority of these fractures, particularly in younger children who have tremendous remodeling potential because of the proximal humerus physis contributing approximately 80% of the bone’s longitudinal growth. This remodeling allows even significantly displaced fractures to heal well without surgery.
Nonoperative treatment typically involves immobilization with a sling and swathe or a shoulder immobilizer and, in some cases, a hanging arm cast may be used to provide gentle traction. Immobilization periods generally range from two to four weeks depending on the patient’s age, with neonates requiring shorter durations. Follow-up is guided by clinical symptoms and radiographic evidence of healing. Operative management is reserved mainly for older children and adolescents who have less growth and remodeling potential, and when fractures are significantly displaced or involve associated injuries, such as open fractures, neurovascular compromise, or polytrauma.36
Generally, clavicle fractures are managed conservatively, with nonoperative treatment being the preferred approach in most cases. Nonoperative management typically involves immobilization using a supportive sling, collar and cuff, or a figure-of-eight bandage for several weeks, depending on the severity of the fracture, the child’s age, and pain levels. Outcomes of nonoperative treatment usually are satisfactory, with low rates of nonunion and malunion, although adolescents might experience longer recovery times and delayed union compared to younger children.
Operative treatment, similar to humeral fractures, is reserved for specific indications, such as open fractures, significantly displaced fractures, fractures with marked shortening, floating shoulder injuries, neurovascular compromise, or cases involving polytrauma.37
AC joint injuries are classified using the Rockwood system (see Table 2), which divides the injuries into six types based on the extent and direction of clavicle displacement and the status of the ligaments around the joint and help to guide management. Type I injuries involve a simple sprain of the AC ligament without displacement. Type II injuries are a complete disruption of the AC ligament but with an intact coracoclavicular ligament and slight displacement. Type III injuries involve complete disruption of both AC and coracoclavicular (CC) ligaments with displacement of the clavicle up to 100% of the CC distance. Type IV injuries are characterized by posterior displacement of the clavicle into or through the trapezius muscle. Type V injuries show severe displacement, more than 100%, with marked disruption of the deltotrapezial fascia. Type VI injuries are rare and involve inferior displacement of the clavicle beneath the coracoid process.10,27
Table 2. Rockwood Classification of AC Joint Injuries |
Type I
Type II
Type III
Type IV
Type V
Type VI
|
AC: acromioclavicular CC: coracoclavicular Adapted from: Sirin E, Aydin N, Mert Topkar O. Acromioclavicular joint injuries: Diagnosis, classification and ligamentoplasty procedures. EFORT Open Rev. 2018;3(7):426-433. |
Treatment varies according to the injury type. Types I and II injuries usually are managed nonoperatively with immobilization, pain control, and gradual rehabilitation. Most patients recover fully with this approach within a few weeks to months. Type III injuries are more controversial; many patients are initially treated nonoperatively, and outcomes can be good, but surgical treatment may be considered in athletes or patients who have persistent symptoms or require heavy use of the shoulder. Types IV, V, and VI injuries generally are treated surgically because of the significant displacement and soft tissue disruption. Surgery aims to restore the joint’s anatomy and stability, often through fixation or ligament reconstruction techniques. The choice of surgical method depends on chronicity, surgeon preference, and through shared decision-making.10,27
Suspected anterior dislocations are managed with closed reduction in the emergency department, with pre-reduction radiographs recommended in patients with open growth plates to exclude proximal humeral physeal fractures. Historically, first-time dislocations were treated nonoperatively with immobilization followed by physical therapy. However, children and adolescents, especially those aged 14 to 18 years, exhibit a high rate of recurrent instability, reported between 56% and 96% after initial dislocation episodes. Surgical intervention often is considered for recurrent instability or in high-risk patients. Arthroscopic Bankart repair commonly is employed in pediatric and adolescent populations and yields excellent outcomes with high rates of return to sport.29,38
After initial treatment, a structured rehabilitation program focusing on restoring range of motion, strength, and stability is vital. Physical therapy may involve specific exercises to improve shoulder mobility and to strengthen the rotator cuff and scapular stabilizers. Gradual return to sports and activities should be carefully monitored and guided by criteria such as the absence of pain and full functional recovery. Overall, a multidisciplinary approach, involving pediatric orthopedic specialists, physical therapists, and primary care providers, is essential to ensure optimal outcomes and safe return to activities for young athletes.10
Disposition
The disposition of pediatric trauma patients depends on the severity of their injuries, with conditions such as head trauma (concussion, intracranial hemorrhage, skull fracture), thoracic injuries (pneumothorax, hemothorax, rib fractures), abdominal trauma (solid organ injury), complex fractures, penetrating injuries, and shock often necessitating admission, surgical evaluation, or intensive care. Management in these cases is multidisciplinary and may require pediatric intensive care unit (PICU) support.9,39
After ruling out life-threatening injuries, ED providers can consider outpatient management for orthopedic injuries without neurovascular injury, with appropriate pain control, with close primary care and specialty follow-up, and with appropriate splinting and/or sling application.
Additional considerations include psychological assessments for children involved in traumatic incidents, since admissions may be indicated for those showing signs of significant emotional distress or post-traumatic stress. Management of pediatric post-traumatic stress disorder (PTSD) following trauma emphasizes early identification and timely intervention using evidence-based approaches. Routine screening for acute stress symptoms during or soon after hospitalization is essential, as highlighted by updated American College of Surgeons guidelines requiring pediatric trauma centers to implement protocols for psychological screening and referral.39,40
Summary
Pediatric shoulder injuries are a significant concern because of the high participation of youth in sports and physical activities. The epidemiology reveals a wide range in prevalence, with injuries commonly occurring in both contact and overhead repetitive motion sports. The most frequent types of injuries include soft tissue injuries, apophysitis, shoulder instability, dislocations, and bony fractures of the clavicle and proximal humerus, all varying by age and skeletal maturity.
Risk factors for these injuries encompass both intrinsic factors, such as muscular weakness, scapular dyskinesia, strength imbalances, and multidirectional instability, and extrinsic factors, including the mechanism of injury, training load increases, and type of sport played. Overhead athletes, particularly females in sports such as volleyball and softball, are at increased risk because of repetitive use and specific biomechanical demands.1-5,7,10,41
Clinical evaluation begins with a systematic primary survey following ATLS principles to identify life-threatening conditions, followed by detailed history-taking and physical examination including inspection, palpation, range of motion assessment, strength testing.9-12 Imaging modalities should be chosen with consideration of radiation exposure in children, adhering to pediatric-specific guidelines to optimize diagnostic utility while minimizing risk.13-17
Psychological assessment and support are vital components of comprehensive care, especially for children exposed to traumatic events, to mitigate post-traumatic stress.39,40
Understanding the unique aspects of pediatric shoulder anatomy, injury mechanisms, clinical presentation, and evidence-based management is essential for optimizing outcomes and facilitating safe return to sport and daily activities in pediatric populations. Continued research and adherence to updated clinical guidelines remain important for enhancing prevention, diagnosis, and treatment strategies.
Jonathon Stewart, MD, is Emergency Medicine Resident, Boonshoft School of Medicine, Wright State University, Dayton, OH.
Vincent Marsh, MD, FACEP, Maj ANG, is Clinical Professor of Emergency Medicine, Boonshoft School of Medicine, Wright State University, Dayton, OH.
References
1. Gibson ES, Cairo A, Räisänen AM, et al. The epidemiology of youth sport-related shoulder injuries: A systematic review. Transl Sports Med. 2022;2022:8791398.
2. Ben Kibler W, Lockhart JW, Cromwell R, Sciascia A. Managing scapular dyskinesis. Phys Med Rehabil Clin N Am. 2023;34(2):427-451.
3. Ben Kibler W, Sciascia AD. Current concepts: Scapular dyskinesis. Br J Sports Med. 2010;44(5):300–5.
4. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641-661.
5. Kibler WB, Ludewig PM, McClure PW, et al. Scapula summit 2009. J Orthop Sports Phys Ther. 2009;39(11):A1–A13.
6. Castonguay J, Hook J, Delgado I, et al. Remote spinal accessory nerve palsy as a cause for scapular dyskinesia in an adolescent baseball pitcher. Int J Case Rep Surg. 2024;6(1):04-06.
7. Steele MC, Lavorgna TR, Ierulli VK, Mulcahey MK. Risk factors for shoulder injuries in female athletes playing overhead sports: A systematic review. Sports Health. 2025;17(3):512-522.
8. Farooq M, Belair JA, Desai V. Pediatric shoulder girdle. Semin Musculoskelet Radiol. 2024;28(4):384-395.
9. American College of Surgeons Committee on Trauma. Advanced Trauma Life Support for You: Student Course Manual. 10th ed. American College of Surgeons; 2018.
10. Abdelgawad A, Naga O, Abdou M, eds. Pediatric Orthopedics and Sports Medicine: A Handbook for Primary Care Physicians. Second edition. Springer; 2021.
11. Bi AS, Jazrawi LM, Cohen SB, Erickson BJ. The physical examination of the throwing shoulder. Clin Sports Med. 2025;44(2):113-128.
12. Cotter EJ, Hannon CP, Christian D, et al. Comprehensive examination of the athlete’s shoulder. Sports Health. 2018;10(4):366-375.
13. American College of Radiology, Society for Pediatric Radiology, and Society of Skeletal Radiology. ACR–SPR–SSR Practice Parameter for the Performance of Radiography of the Extremities. American College of Radiology, revised 2023. https://gravitas.acr.org/PPTS/GetDocumentView?docId=12
14. Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: A catalog. Radiology. 2008;248(1):254-263.
15. RadiologyInfo.org. X-ray Safety. https://www.radiologyinfo.org
16. American College of Radiology, American Society of Emergency Radiology, Society of Computed Body Tomography and Magnetic Resonance, Society for Pediatric Radiology. ACR–ASER–SCBT-MR–SPR practice parameter for the performance of pediatric computed tomography (CT). Revised 2019. Amended 2023. https://gravitas.acr.org/PPTS/GetDocumentView?docId=77
17. American College of Radiology, Society of Pediatric Radiology, and Society of Skeletal Radiology. ACR–SPR–SSR Practice Parameter for the Performance and Interpretation of Magnetic Resonance Imaging (MRI) of the Shoulder. 2024. https://gravitas.acr.org/PPTS/GetDocumentView?docId=45
18. Shioji N, Everett T, Suzuki Y, Aoyama K. Pediatric sedation using dexmedetomidine and remimazolam for magnetic resonance imaging. J Anesth. 2022;36(1):1-4.
19. Stern J, Agarwal A, Pozun A. Pediatric Procedural Sedation. In: StatPearls. StatPearls Publishing; March 22, 2025.
20. Piccolo CL, Galluzzo M, Ianniello S, et al. Pediatric musculoskeletal injuries: Role of ultrasound and magnetic resonance imaging. Musculoskelet Surg. 2017;101(Suppl 1):85-102.
21. Kim WG, Laor T, Jarrett DY. Physeal injuries of the clavicle: Pediatric counterparts to adult acromioclavicular and sternoclavicular joint separations. Pediatr Radiol. 2023;53(8):1513-1525.
22. Markes AR, Garcia-Lopez E, Halvorson RT, Swarup I. Management of displaced midshaft clavicle fractures in pediatrics and adolescents: Operative vs nonoperative treatment. Orthop Res Rev. 2022;14:373-381.
23. Fonacier FS, Chan HK, Ugalde I. Pediatric scapular fractures and associated injuries following blunt chest trauma. Am J Emerg Med. 2022;52:196-199.
24. Gonzalez-Morgado D, Vargas Meouchi EA, Soza Leiva D, et al. Acromial physeal fracture in an adolescent: A case report and literature review. JSES Int. 2023;8(1):6-10.
25. Myers NL, Kennedy SM, Arnold AJ, et al. A narrative review of little league shoulder: Proximal humeral physis widening is only one piece of the puzzle, it is time to consider posterior glenoid dysplasia. JSES Int. 2024;8(4):724-733.
26. Pennock AT, Dwek J, Levy E, et al. Shoulder MRI abnormalities in asymptomatic Little League baseball players. Orthop J Sports Med. 2018;6(2):2325967118756825.
27. Kelley N, Tuttle M, Sylvia SM, et al. Acromioclavicular joint injuries in sport. Curr Sports Med Rep. 2023;22(3):91-99.
28. Park R, Wood KS. Case report: Pediatric posterior shoulder dislocation. JSES Rev Rep Tech. 2021;1(2):130-134.
29. Kay J, Heyworth BE, Milewski MD, Kramer DE. Pediatric and adolescent shoulder instability. Curr Rev Musculoskelet Med. 2023;16(7):263-273.
30. Franklin CC, Weiss JM. The natural history of pediatric and adolescent shoulder dislocation. J Pediatr Orthop. 2019;39(6, Suppl 1):S50-S52.
31. Warner T, Kay J, McInnis S, Heyworth BE. Risk factors for recurrent instability after arthroscopic Bankart repair in pediatric and adolescent patients: A systematic review. Am J Sports Med. 2025;53(6):1494-1504.
32. Cannamela P, Cutler H, Sohn G, et al. Atypical shoulder instability patterns in adolescents following traumatic anterior shoulder dislocation. Am J Sports Med. 2023;51(8):2018-2022.
33. Johnson DJ, Tadi P. Multidirectional Shoulder Instability. In: StatPearls. StatPearls Publishing; July 3, 2023.
34. Manan MR, Rahman S, Komer L, et al. A multispecialty approach to the identification and diagnosis of nonaccidental trauma in children. Cureus. 2022;14(7):e27276.
35. Casadei K, Kiel J. Proximal Humeral Epiphysiolysis. In: StatPearls. StatPearls Publishing; April 3, 2023.
36. Kim AE, Chi H, Niknam K, Swarup I. Management of pediatric proximal humerus fractures. J Pediatr Soc North Am. 2024;5(1):580.
37. van der Water L, Macken AA, Eygendaal D, van Bergen CJA. Pediatric clavicle fractures and congenital pseudarthrosis unraveled. Children (Basel). 2022;9(1):49.
38. Kay J, Heyworth BE, Bae DS, et al. Arthroscopic Bankart repair for anterior glenohumeral instability in 488 adolescents between 2000 and 2020: Risk ractors for subsequent recurrent instability requiring revision stabilization. Am J Sports Med. 2024;52(9):2331-2339.
39. Smithson KB, Parham SG, Mears SC, et al. Transfers of pediatric patients with isolated injuries to a rural Level 1 Orthopedic Trauma Center in the United States: Are they all necessary? Arch Orthop Trauma Surg. 2022;142(4):625-631.
40. Fuchs J, Zwemer E, Gillespie A, et al. Making trauma less traumatic: Implementing inpatient pediatric screening of acute stress symptoms. Hosp Pediatr. 2023;13(8):702-710.
41. Levine RH, Thomas A, Nezwek TA, Waseem M. Salter-Harris Fracture. In: StatPearls. StatPearls Publishing; Aug. 10, 2023.