Clinician
Blog articles for clinicians and other medical professionals.
Implantable Cardioverter Defibrillator Complications and Management
May 14th, 2025
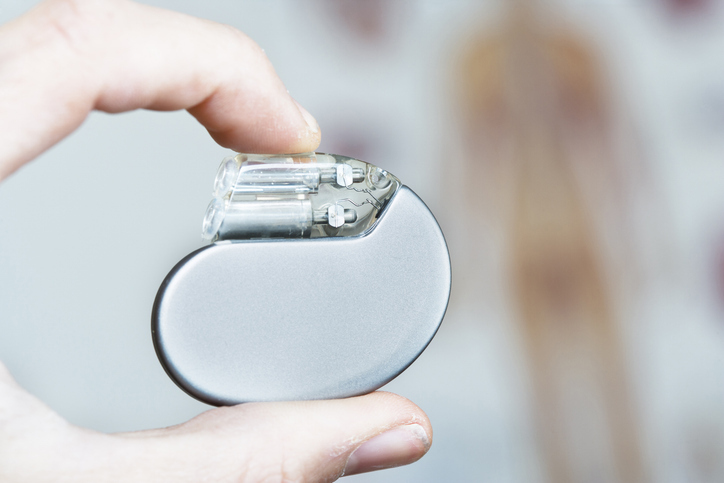
Implantable cardioverter defibrillators (ICDs), used primarily to treat life-threatening ventricular arrhythmias, increasingly are common among emergency department patients. ICDs offer life-saving therapy through anti-tachycardia pacing or defibrillation shocks. They are used in conditions such as cardiac arrest history, heart failure with reduced ejection fraction (≤35%), hypertrophic cardiomyopathy, and adult congenital heart disease. Several types of ICDs exist — single-chamber, dual-chamber, and biventricular — as well as subcutaneous models that provide shocks without pacing capabilities.
Despite their benefits, ICDs carry a significant complication burden, affecting 9% to 11% of patients within a year of implantation. Younger patients, women, and Black individuals are at elevated risk. Implantation frequency also influences outcomes — higher-volume centers and operators see fewer complications.
Early and Procedural Complications
Common mechanical issues include bleeding, pneumothorax, hemothorax, and cardiac perforation. Pocket hematomas — collections of blood at the implantation site — are especially prevalent and may necessitate drainage or surgical management. Hemorrhagic complications are exacerbated by anticoagulation or antiplatelet therapy and are more frequent with subpectoral device placements and in patients with low body mass index.
Pneumothorax occurs in about 1% of patients, more often in women and those with chronic obstructive pulmonary disease. Cardiac perforation is rare but potentially life-threatening, with atrial wall perforation more common than ventricular. Prompt imaging, including echocardiography, is essential for diagnosis, and treatment ranges from observation to emergent surgery depending on symptom severity.
Long-Term and Functional Complications
Twiddler’s syndrome — device manipulation by the patient — can cause lead dislodgement and device malfunction. Venous thrombosis or stenosis, especially in the subclavian and brachiocephalic veins, may result from lead placement and often remains asymptomatic. In severe cases, superior vena cava syndrome may develop and requires transvenous lead extraction (TLE) or venoplasty.
Device-related infections, occurring in 1% to 2% of cases, can range from superficial pocket infections to systemic endocarditis. Management typically involves antibiotics, and, often, device removal, especially in systemic infections. TLE is necessary in many infected cases but carries a risk of stroke, valvular damage, or vascular injury.
Functional issues include magnetic resonance imaging (MRI) incompatibility, lead failure, and inappropriate shocks. Some devices are MRI-compatible, but older models are not, posing risks during imaging. Lead failure can impair sensing or shock delivery and is more likely in younger, active patients. Inappropriate shocks arise from misinterpretation of electrical signals or electromagnetic interference, potentially causing patient harm or distress.
Device Maintenance and Alternatives
Battery depletion, typically occurring every four to seven years, necessitates generator replacement, which increases infection risk. Reoperation rates are higher with dual-chamber devices, although these more complicated devices may continue to confer greater benefit to patients who experience atrial arrhythmias. In patients not receiving therapeutic intervention from an ICD, replacement may not be indicated because of surgical risk.
Wearable cardiac defibrillators provide temporary protection in patients not eligible for ICDs because of transient conditions or recent device explantation. Adherence to WCD use is crucial, particularly in older populations with higher rates of arrhythmic events.
Conclusion
ICDs significantly improve survival in select cardiac patients but come with a notable risk of complications. Emergency providers must be well-versed in the diagnosis and management of these issues, ranging from minor procedural concerns to life-threatening device failures.
To learn more about the specifics of ICD implantation and its associated complications, click here.